An overview of Diabetes
What is Diabetes?
Diabetes is a condition that happens when your blood sugar (glucose) is too high. It develops when your pancreas doesn’t make enough insulin or any at all, or when your body isn’t responding to the effects of insulin properly.
When glucose is in your bloodstream, it needs help — a “key” — to reach its final destination. This key is insulin (a hormone). If your pancreas isn’t making enough insulin or your body isn’t using it properly, glucose builds up in your bloodstream, causing high blood sugar (hyperglycemia).
Types of Diabetes?
Type 1 diabetes : This type is an autoimmune disease in which your immune system attacks and destroys insulin-producing cells in your pancreas for unknown reasons. Up to 10% of people who have diabetes have Type 1. It’s usually diagnosed in children and young adults, but it can develop at any age.
Type 2 diabetes : With this type, your body doesn’t make enough insulin and/or your body’s cells don’t respond normally to the insulin (insulin resistance). This is the most common type of diabetes. It mainly affects adults, but children can have it as well.
Prediabetes : This type is the stage before Type 2 diabetes. Your blood glucose levels are higher than normal but not high enough to be officially diagnosed with Type 2 diabetes.
Gestational diabetes : This type develops in some people during pregnancy. Gestational diabetes usually goes away after pregnancy. However, if you have gestational diabetes, you’re at a higher risk of developing Type 2 diabetes later in life.
Causes of Diabetes
Too much glucose circulating in your bloodstream causes diabetes, regardless of the type. However, the reason why your blood glucose levels are high differs depending on the type of diabetes.
Insulin resistance : Type 2 diabetes mainly results from insulin resistance. Insulin resistance happens when cells in your muscles, fat and liver don’t respond as they should to insulin. Several factors and conditions contribute to varying degrees of insulin resistance, including obesity, lack of physical activity, diet, hormonal imbalances, genetics and certain medications.
Autoimmune disease : Type 1 diabetes and LADA happen when your immune system attacks the insulin-producing cells in your pancreas.
Hormonal imbalances : During pregnancy, the placenta releases hormones that cause insulin resistance. You may develop gestational diabetes if your pancreas can’t produce enough insulin to overcome the insulin resistance. Other hormone-related conditions like acromegaly and Cushing syndrome can also cause Type 2 diabetes.
Pancreatic damage : Physical damage to your pancreas — from a condition, surgery or injury — can impact its ability to make insulin, resulting in Type 3c diabetes.
Genetic mutations : Certain genetic mutations can cause MODY and neonatal diabetes.
Long-term use of certain medications can also lead to Type 2 diabetes, including HIV/AIDS medications and corticosteroids.
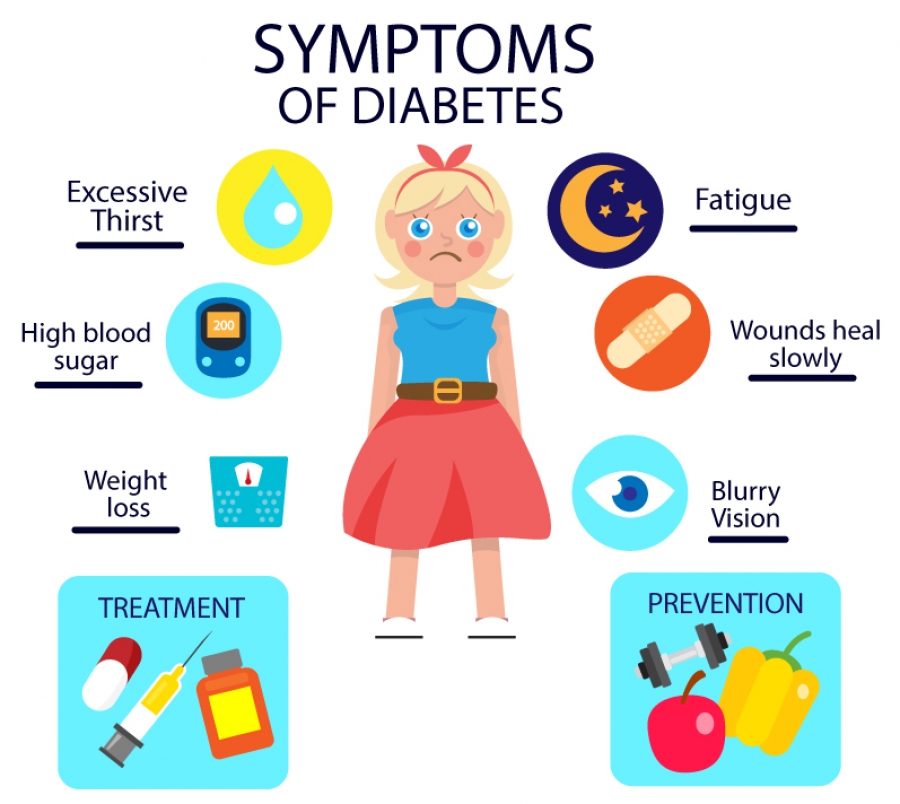
Signs and symptoms of Diabetes?
Diabetes symptoms depend on how high your blood sugar is. Some people, especially if they have prediabetes, gestational diabetes or type 2 diabetes, may not have symptoms. In type 1 diabetes, symptoms tend to come on quickly and be more severe.
Some of the symptoms of type 1 diabetes and type 2 diabetes are:
1. Feeling more thirsty than usual.
2. Urinating often.
3. Losing weight without trying.
4. Presence of ketones in the urine. Ketones are a byproduct of the breakdown of muscle and fat that happens when there's not enough available insulin.
5. Feeling tired and weak.
6. Feeling irritable or having other mood changes.
7. Having blurry vision.
8. Having slow-healing sores.
9. Getting a lot of infections, such as gum, skin and vaginal infections.
How can I prevent diabetes?
You can’t prevent autoimmune and genetic forms of diabetes. But there are some steps you can take to lower your risk for developing prediabetes, Type 2 diabetes and gestational diabetes, including:
1. Eat a healthy diet, such as the Mediterranean diet.
2. Get physically active. Aim for 30 minutes a day at least five days a week.
3. Work to achieve a weight that’s healthy for you.
4. Manage your stress.
5. Limit alcohol intake.
6. Get adequate sleep (typically 7 to 9 hours) and seek treatment for sleep disorders.
7. Quit smoking.
8. Take medications as directed by your healthcare provider to manage existing risk factors for heart disease.
It’s important to note that there are some diabetes risk factors you can’t change, such as your genetics/family history, age and race. Know that Type 2 diabetes is a complex condition that involves many contributing factors.
How is Diabetes diagnosed?
Healthcare providers diagnose diabetes by checking your glucose level in a blood test. Three tests can measure your blood glucose level:
Fasting blood glucose test: For this test, you don’t eat or drink anything except water (fast) for at least eight hours before the test. As food can greatly affect blood sugar, this test allows your provider to see your baseline blood sugar.
Random blood glucose test: “Random” means that you can get this test at any time, regardless of if you’ve fasted.
A1c: This test, also called HbA1C or glycated hemoglobin test, provides your average blood glucose level over the past two to three months.
How is Diabetes managed or treated?
Diabetes is a complex condition, so its management involves several strategies. In addition, diabetes affects everyone differently, so management plans are highly individualized.
The four main aspects of managing diabetes include:
Blood sugar monitoring : Monitoring your blood sugar (glucose) is key to determining how well your current treatment plan is working. It gives you information on how to manage your diabetes on a daily — and sometimes even hourly — basis. You can monitor your levels with frequent checks with a glucose meter and finger stick and/or with a continuous glucose monitor (CGM). You and your healthcare provider will determine the best blood sugar range for you.
Oral diabetes medications : Oral diabetes medications (taken by mouth) help manage blood sugar levels in people who have diabetes but still produce some insulin — mainly people with Type 2 diabetes and prediabetes. People with gestational diabetes may also need oral medication. There are several different types. Metformin is the most common.
Insulin : People with Type 1 diabetes need to inject synthetic insulin to live and manage diabetes. Some people with Type 2 diabetes also require insulin. There are several different types of synthetic insulin. They each start to work at different speeds and last in your body for different lengths of time. The four main ways you can take insulin include injectable insulin with a syringe (shot), insulin pens, insulin pumps and rapid-acting inhaled insulin.
Diet : Meal planning and choosing a healthy diet for you are key aspects of diabetes management, as food greatly impacts blood sugar. If you take insulin, counting carbs in the food and drinks you consume is a large part of management. The amount of carbs you eat determines how much insulin you need at meals. Healthy eating habits can also help you manage your weight and reduce your heart disease risk.
Exercise : Physical activity increases insulin sensitivity (and helps reduce insulin resistance), so regular exercise is an important part of management for all people with diabetes.
Frequently Asked Questions About Diabetes
Diabetes is common. Approximately 37.3 million people in the United States have diabetes, which is about 11% of the population. Type 2 diabetes is the most common form, representing 90% to 95% of all diabetes cases. About 537 million adults across the world have diabetes. Experts predict this number will rise to 643 million by 2030 and 783 million by 2045.
If you haven’t been diagnosed with diabetes, you should see a healthcare provider if you have any symptoms of diabetes, such as increased thirst and frequent urination.