An overview of Covid 19
What is COVID-19?
COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly. Over one million people have died from COVID-19 in the United States.COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia. COVID-19 may attack more than your lungs and respiratory system. Other parts of your body may also be affected by the disease. Most people with COVID-19 have mild symptoms, but some people become severely ill.Some people including those with minor or no symptoms will develop Post-COVID Conditions – also called “Long COVID.”
Causes of Covid-19
Infection with severe acute respiratory syndrome coronavirus 2, also called SARS-CoV-2, causes coronavirus disease 2019 (COVID-19).
The virus that causes COVID-19 spreads easily among people. Data has shown that the COVID-19 virus spreads mainly from person to person among those in close contact. The virus spreads by respiratory droplets released when someone with the virus coughs, sneezes, breathes, sings or talks. These droplets can be inhaled or land in the mouth, nose or eyes of a person nearby.
Sometimes the COVID-19 virus can spread when a person is exposed to very small droplets or aerosols that stay in the air for several minutes or hours — called airborne transmission.
The virus also can spread if you touch a surface with the virus on it and then touch your mouth, nose or eyes. But the risk is low.
The COVID-19 virus can spread from someone who is infected but has no symptoms. This is called asymptomatic transmission. The COVID-19 virus also can spread from someone who is infected but hasn't developed symptoms yet. This is called presymptomatic transmission.
It's possible to get COVID-19 more than once.
1. Close contact with someone who has COVID-19, especially someone with symptoms.
2. Being coughed or sneezed on by an infected person.
3. Being near an infected person when in an indoor space with poor airflow.
Risk factors for serious COVID-19 illness
Some people are at a higher risk of serious COVID-19 illness than others. This includes people who are older, and the risk increases with age.
People with existing medical conditions also may have a higher risk of serious illness. This includes people who have:
1. Sickle cell disease or thalassemia.
2. Serious heart diseases, such as heart failure, coronary artery disease or cardiomyopathy, and possibly high blood pressure.
3. Chronic kidney, liver or lung diseases
People with dementia or Alzheimer's are also at higher risk, as are people with brain and nervous system conditions such as stroke. Smoking increases the risk of serious COVID-19 illness. And people with body mass index in the overweight category or obese category may have an increased risk as well.
Other medical conditions that may increase the risk of serious illness from COVID-19 include:
1. Cancer.
2. Type 1 or type 2 diabetes
3. Weakened immune system from solid organ transplants or bone marrow transplants,some medicines, or HIV.
4. Pregnancy.
5. Down syndrome.
6. Substance use disorders.
This list is not complete. Other medical conditions may increase your risk of serious illness from COVID-19.
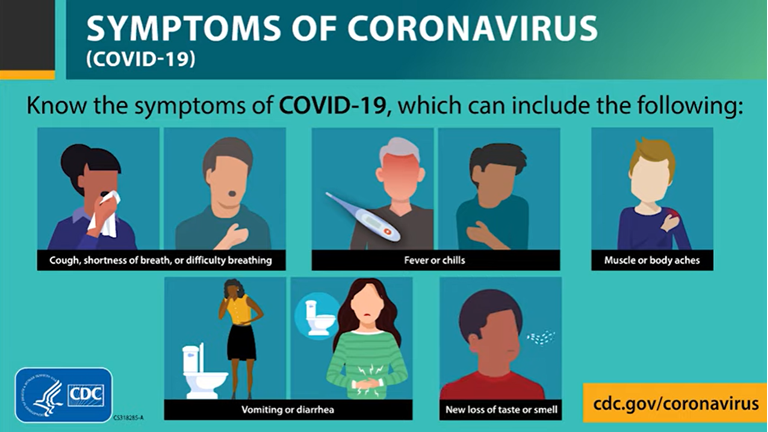
Signs and symptoms of Covid-19
People with COVID-19 have had a wide range of symptoms reported – ranging from mild symptoms to severe illness. Symptoms may appear 2-14 days after exposure to the virus. Anyone can have mild to severe symptoms. Possible symptoms include:
1. Fever or chills
2. Cough
3. Shortness of breath or difficulty breathing
4. Fatigue
5. Muscle or body aches
6. Headache
7. New loss of taste or smell
8. Sore throat
9. Congestion or runny nose
10. Nausea or vomiting
11. Diarrhea
This list does not include all possible symptoms. Symptoms may change with new COVID-19 variants and can vary depending on vaccination status. CDC will continue to update this list as we learn more about COVID-19. Older adults and people who have underlying medical conditions like heart or lung disease or diabetes are at higher risk for getting very sick from COVID-19.
Preventive measures against Covid-19
Follow the guidelines to help protect yourself from contracting and transmitting SARS-CoV-2.
Lifestyle changes you can make to help prevent Covid-19 include:
1. Wash your hands frequently and carefully
Use warm water and soap and rub your hands for at least 20 seconds. Work the lather to your wrists, between your fingers, and under your fingernails. You can also use an antibacterial and antiviral soap.
Use hand sanitizer when you cannot wash your hands properly. Rewash your hands several times a day, especially after touching anything, including your phone or laptop.
2. Avoid touching your face
SARS-CoV-2 can live on some surfaces for up to 72 hours. You can get the virus on your hands if you touch a surface like:
gas pump handle
your cell phone
a doorknob
Avoid touching any part of your face or head, including your mouth, nose, and eyes. Also avoid biting your fingernails. This can give SARS-CoV-2 a chance to go from your hands into your body.
3. Stop shaking hands and hugging people — for now
Similarly, avoid touching other people. Skin-to-skin contact can transmit SARS-CoV-2 from one person to another.
4. Don’t share personal items
Do not share personal items like:
phones
makeup
combs
It’s also important not to share eating utensils and straws. Teach children to recognize their reusable cup, straw, and other dishes for their own use only.
5. Cover your mouth and nose when you cough and sneeze
SARS-CoV-2 is found in high amounts in the nose and mouth. This means it can be carried by air droplets to other people when you cough, sneeze, or talk. It can also land on hard surfaces and stay there for up to 3 days.
Use a tissue or sneeze into your elbow to keep your hands as clean as possible. Wash your hands carefully after you sneeze or cough, regardless.
6. Clean and disinfect surfaces
Use alcohol-based disinfectants to clean hard surfaces in your home like:
countertops
door handles
furnitures
toys
Also, clean your phone, laptop, and anything else you use regularly several times a day.
Disinfect areas after you bring groceries or packages into your home.
Use white vinegar or hydrogen peroxide solutions for general cleaning in between disinfecting surfaces.
7. Take physical (social) distancing seriously
If you’re carrying the SARS-CoV-2 virus, it’ll be found in high amounts in your spit (sputum). This can happen even if you don’t have symptoms.
Physical (social) distancing, also means staying home and working remotely when possible.
If you must go out for necessities, keep a distance of 6 feet (2 m) from other people. You can transmit the virus by speaking to someone in close contact to you.
8. Do not gather in groups
Being in a group or gathering makes it more likely that you’ll be in close contact with someone.
This includes avoiding all religious places of worship, as you may have to sit or stand too close to another congregant. It also includes not congregating at parks or beaches.
9. Avoid eating or drinking in public places
Now is not the time to go out to eat. This means avoiding restaurants, coffee shops, bars, and other eateries.
The virus can be transmitted through food, utensils, dishes, and cups. It may also be temporarily airborne from other people in the venue.
You can still get delivery or takeaway food. Choose foods that are thoroughly cooked and can be reheated.
High heat (at least132°F/56°C, according to one recent, not-yet-peer-reviewed lab study) helps to kill coronaviruses.
This means it may be best to avoid cold foods from restaurants and all food from buffets and open salad bars.
10. Wash fresh groceries
Wash all produce under running water before eating or preparing.
The CDC and the FDA do not recommend using soap, detergent, or commercial produce wash on things like fruits and vegetables. Be sure to wash hands before and after handling these items.
11. Wear a (homemade) mask
The Centers for Disease Control and Prevention (CDC) that almost everyone wears a cloth face mask in public settings where physical distancing may be difficult, such as grocery stores.
When used correctly, these masks can help prevent people who are asymptomatic or undiagnosed from transmitting SARS-CoV-2 when they breathe, talk, sneeze, or cough. This, in turn, slows the transmission of the virus.
The CDC’s website provides instructionsan for making your own mask at home, using basic materials such as a T-shirt and scissors.
Some pointers to keep in mind:
Wearing a mask alone will not prevent you from getting a SARS-CoV-2 infection. Careful handwashing and physical distancing must also be followed.
Cloth masks aren’t as effective as other types of masks, such as surgical masks or N95 respirators. However, these other masks should be reserved for healthcare workers and first responders.
Wash your hands before you put on your mask.
Wash your mask after each use.
You can transfer the virus from your hands to the mask. If you’re wearing a mask, avoid touching the front of it.
You can also transfer the virus from the mask to your hands. Wash your hands if you touch the front of the mask.
A mask shouldn’t be worn by a child under 2 years old, a person who has trouble breathing, or a person who can’t remove the mask on their own.
12. Self-quarantine if sick
Call your doctor if you have any symptoms. Stay home until you recover. Avoid sitting, sleeping, or eating with your loved ones even if you live in the same home.
Wear a mask and wash your hands as much as possible. If you need urgent medical care, wear a mask and let them know you may have COVID-19.
How Is Covid-19 Diagnosed?
If you develop symptoms of coronavirus disease 2019 (COVID-19) or you'vebeen exposed to the COVID-19 virus, contact your health care team.Also let your health care team know if you've had close contact withanyone who has been diagnosed with COVID-19.
Factors used to decide whether to test you for the virus that causes COVID-19may differ depending on where you live. Depending on your location, youmay need to be screened by your clinic to determine if testing ispropriate and available.
In the U.S., your health care team will determine whether to conduct tests for thevirus that causes COVID-19 based on your symptoms, as well aswhether you have had close contact with someone diagnosed withCOVID-19.
You also may be tested if you are at higher risk of seriousillness or you are going to have a medical procedure.
If you have had close contact with someone withCOVID-19 but you'vehad COVID-19 in the past month, you don't need to be tested.
If you've been fully vaccinated and you've had close contact with someonewith COVID-19, gettested five days after you've had contact with that person.
To test for the COVID-19 virus, a health care professional takes a sample from the nose(nasopharyngeal swab), throat (throat swab) or saliva. The samples are thensent to a lab for testing. If you're coughing up sputum, that may be sent for testing.
At-home tests for COVID-19 areavailable at many pharmacies. Some of these tests require a prescription, but some,called antigen tests, are available without a prescription. Antigen tests are not asreliable as the test done in a lab. But it is a fast and easy way to test yourself assoon as you have symptoms or at least five days after you've been exposed to the virusthat causes COVID-19.
If you test negative, you can take the test a second time a few dayslater to help ensure your test results are accurate. The accuracy ofeach of these tests varies. So a negative test does not completelyrule out having the COVID-19 virus.
Only get an at-home test that's authorized by the FDAor approved by your health care professional or local health department.
Treatment for Covid-19
Currently, a few medicines have been approved to treatCOVID-19. No cure isavailable for COVID-19. Antibiotics aren'teffective against viral infections such as COVID-19.Researchers are testing a variety of possible treatments.
The FDA has approved the antiviral medicine remdesivir (Veklury) to treat COVID-19 in adults and children who are age 12 and older in the hospital. Remdesivir may be prescribed for people who are hospitalized with COVID-19 and need supplemental oxygen or have a higher risk of serious illness. It's given through a needle in the vein.
Paxlovid is another medicine approved to treat COVID-19 in adults. It includes nirmatrelvir — a drug that blocks the activity of a specific enzyme needed for the virus that causes COVID-19to replicate — and an antiviral drug called ritonavir that helps slow the breakdown of nirmatrelvir. Paxlovid continues to be available under emergency use authorization to treat mild to moderate COVID-19 in people age 12 and older who are at higher risk of serious illness. Paxlovid pills are taken by mouth.
The FDA also has approved the rheumatoid arthritis drugs baricitinib (Olumiant) and tocilizumab (Actemra) to treat COVID-19 in some cases. Baricitinib is a pill that seems to work against COVID-19 by reducing inflammation and having antiviral activity. Tocilizumab is an injection. It seems to work against COVID-19 by reducing inflammation. Both medicines may be used in people in the hospital with COVID-19 who are on mechanical ventilators or need supplemental oxygen.
The FDA has authorized another drug called molnupiravir (Lagevrio) to treat mild to moderate COVID-19 in adults who are at higher risk of serious illness and who aren't able to take other treatment options. The medicine is taken by mouth as a pill.
The U.S. National Institutes of Health has recommended the corticosteroid dexamethasone for people hospitalized with severe COVID-19 who are on supplemental oxygen or need mechanical ventilation. Other corticosteroids, such as prednisone, methylprednisolone (Medrol) or hydrocortisone, may be used if dexamethasone isn't available.
In some cases, the drugs remdesivir, tocilizumab or baricitinib may be given with dexamethasone in people who are on mechanical ventilation or need supplemental oxygen in the hospital.
Other therapies also may be used for people who need oxygen or who are on mechanical ventilation or extracorporeal membrane oxygenation, called ECMO. The immune system suppression drug anakinra (Kineret) was authorized by the FDA for people who need supplemental oxygen. And vilobelimab (Gohibic), a monoclonal antibody, was authorized by the FDA for those who are on mechanical ventilation or ECMO.
The FDA also has authorized COVID-19 convalescent plasma therapy with high antibody levels to treat COVID-19. Convalescent plasma is blood donated by people who've recovered from. Convalescent plasma with high antibodies may be used to help people diagnosed with COVID-19 who have weakened immune systems.
Many people with COVID-19 may have mild illness and can be treated with supportive care. Supportive care is aimed at relieving symptoms and may include:
Pain relievers, such as ibuprofen or acetaminophen.
Cough syrup or medicine.
Rest.
Fluid intake.
There is no evidence that ibuprofen or other nonsteroidal anti-inflammatory drugs (NSAIDS) need to be avoided.
If you have mild symptoms, your health care professional will likely recommend that you recover at home.
You may be given special instructions to monitor your symptoms and to avoid spreading the illness to others. You'll likely be asked to isolate yourself as much as possible from family and pets while you're sick, wear a mask when you're around people and pets, and use a separate bedroom and bathroom.
And keep airflow in your home by opening windows and using air filters when possible.
Your health care team will likely recommend that you stay in home isolation for a period of time except to get medical care. Your health care professional will likely follow up with you regularly.
Follow guidelines from your health care team and local health department about when you can end home isolation.
If you're very ill, you may need to be treated in the hospital.
What are the stages of coronavirus infection?
There are three general phases of infection with SARS-Cov-2, the coronavirus that causes COVID-19.
Incubation period.
This is the time between getting infected and when symptoms appear. In general, you may see symptoms start two to 14 days after infection. The incubation period varies among individuals, and it varies depending on the variant. Even though you do not have symptoms in the incubation period, you can transmit the coronavirus to another person during this stage.
This is why, if you suspect you were exposed to someone with COVID-19, you should self-quarantine, watch for symptoms and consider getting tested four or five days following the exposure. This way, you can help prevent the spread of COVID-19. Please review Centers for Disease Control and Prevention (CDC) guidelines for isolation and quarantine.
Acute COVID-19.
Once symptoms appear, you have entered the acute stage. You may have fever, cough and other COVID-19 symptoms. Active illness can last one to two weeks if you have mild or moderate coronavirus disease, but severe cases can last months. Some people are asymptomatic, meaning they never have symptoms but do have COVID-19.
If you develop symptoms or suspect you are asymptomatically infected, call your health care provider, follow testing guidelines, and follow all isolation and safety guidelines.
COVID-19 recovery.
Post-COVID-19 symptoms, such as lingering cough, on and off fever, weakness, and changes to your senses of smell or taste, can persist for weeks or even months after you recover from acute illness. Persistent symptoms are sometimes known as long COVID-19.
Test results may remain positive for weeks to several months following infection, but this does not necessarily mean you are still infectious. Most people are no longer infectious beyond the recommended isolation precautions period. If you have conditions that cause severe immunosuppression, contact your health care provider to determine how long you should isolate and how to determine when you are no longer potentially infectious to others.
Complications Coronavirus Can Cause
If you have COVID-19, your symptoms may be relatively mild and manageable at home. That’s true for most people. But if you’re older or have another illness such as diabetes or heart disease, you’re more at risk for the serious form of COVID-19.
Some people -- about 1 in 6 -- will have complications, including some that are life-threatening. Many of these complications may be caused by a condition known as cytokine release syndrome or a cytokine storm. This is when an infection triggers your immune system to flood your bloodstream with inflammatory proteins called cytokines. They can kill tissue and damage your organs, including your lungs, heart, and kidneys.
COVID-19 complications may include the following.
Acute Respiratory Failure
When you have acute respiratory failure, your lungs might not pump enough oxygen into your blood or might not take enough carbon dioxide out. Both of these problems can happen at the same time.
Acute respiratory failure has been the leading cause of death for those who have died of COVID-19
Pneumonia
Some who catch the new coronavirus get severe pneumonia in both lungs. COVID-19 pneumonia is a serious illness that can be deadly. When you have pneumonia, the air sacs in your lungs become inflamed, making it harder to breathe.
Images of very ill COVID-19 patients’ lungs show them filled with fluid, pus, and cell debris. In those cases, patients’ bodies weren’t able to transfer oxygen to the blood to keep their systems working properly.
Acute Respiratory Distress Syndrome (ARDS)
Acute respiratory distress syndrome (ARDS) was one of the most common complications of COVID-19.
With ARDS, the lungs are so severely damaged that fluid begins to leak into them. As a result, the body has trouble getting oxygen into the bloodstream. You may need mechanical help to breathe -- such as a ventilatoruntil your lungs recover.
Acute Liver Injury
Most seriously ill patients run the greatest risk of liver damage. It's unclear whether the virus harms the liver or if it happens for another reason, but besides the lungs, the liver usually suffers the biggest injuries from COVID-19.
Acute liver injury and liver failure are life-threatening complications. (“Acute” means it happens suddenly.)
Acute Cardiac Injury
Many hospitalized with COVID-19 have developed heart problems, including arrhythmias and high levels of other cardiac ailments. But it’s not clear whether the virus itself affected patients’ hearts, or if the damage happened simply because the illness caused such stress on their bodies overall.
COVID-19 also may cause cardiac problems that last long after people have recovered from the coronavirus infection.
Secondary Infection
A secondary infection means that you get an infection unrelated to the first problem you had. In this case, it means someone with COVID-19 gets infected with something else.
Sometimes, a person fighting off, or recovering from, a virus gets infected by bacteria. Strep and are common culprits. This can be serious enough to raise the risk of death.
Acute Kidney Injury
This is not a common complication, but if it happens, it’s serious. If your kidneys stop working properly, doctors will start treatment to stop the damage. You might get (in which a machine filters your blood) until your kidneys get back to working normally. But sometimes, the damage doesn’t heal and people get chronic kidney disease, which would need to be managed long-term.
Septic Shock
Sepsis happens when your body’s reaction to an infection misfires. The chemicals released into your bloodstream to battle the illness don’t trigger the right response, and instead your organs are damaged. If the process isn’t stopped, you can go into what’s called septic shock. If your blood pressure drops too much, septic shock can be fatal.
Disseminated Intravascular Coagulation
When you have disseminated intravascular coagulation, or DIC, the body’s blood-clotting response doesn’t work right. Abnormal clots form, which can lead to internal bleeding or organ failure.
DIC is not uncommon among those who have died or COVID.
Blood Clots
A condition called disseminated intravascular coagulation (DIC) causes your body’s blood-clotting response to work differently than it should. Unusual clots form, which can lead to internal bleeding or organ failure and death.
Those hospitalized with COVID have been found to be more likely to develop clots than those hospitalized with the flu. Some were in patients’ legs (deep vein thrombosis or DVT), lungs (pulmonary embolism or PE), or arteries. But none of the patients had DIC.
COVID-19-associated coagulopathy (CAC) is a life-threatening condition caused by the virus. It’s marked by different protein levels in your blood than the ones caused by DIC.
Frequently Asked Questions About COVID-19
Scientists and public health officials are workinghard to identify the source of the SARS-CoV-2 whichis the virus that causes COVID-19. The initialtransmission appeared to be from an animal source,but there has been person-to-person transmission in countries.
From the evidence so far, the virus causing COVID-19can be transmitted in ALL AREAS, including areas withhot and humid weather.
There is no specific cure yet for COVID-19. However,there are many ongoing clinical trials to test variouspotential antivirals. Current management of cases aims torelieve the symptoms while the body’s immune system fightsthe illness.
Currently, the national case management guidelines stipulatethat hydroxychloroquine should only be used in clinical trialsettings, until there is scientific evidence on its efficacyand safety.