An overview of Hepatitis
What is Viral Hepatitis?
Viral hepatitis is the inflammation and damage of liver cells due to infection. There are different types and causes of hepatitis.
The liver is essential for removing toxins from the blood, storing vitamins, and producing hormones along with other functions. Viral hepatitis can disrupt these important processes, causing various health concerns.
Type of Viral Hepatitis?
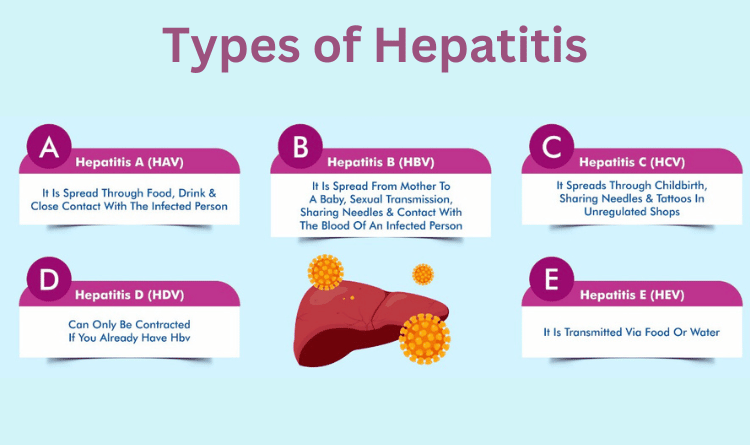
There are five main viruses that cause viral hepatitis, termed A, B, C, D and E. These types are of greatest concern due to their potential to cause illness and, in some cases, life threatening complications.
Each type has different characteristics, and transmission happens differently, but the symptoms tend to be similar.
Hepatitis A
The Centers for Disease Control and Prevention (CDC) estimate around 24,900 new hepatitis A infections each year in the United States.
Overall, the number of U.S. cases has declined during the past 20 years — largely due to immunization — but outbreaks sometimes occur.
People typically contract Hepatitis A from food or water that has come into contact with fecal matter from a person with the virus. It is common in many countries, especially those with ineffective sanitation systems.
Symptoms
A person will typically experience symptoms within 14–28 days. Symptoms include:
1. jaundice
2. fever
3. diarrhea
4. dark-colored urine
5. malaise
6. abdominal pain
7. nausea
8. low appetite
However, many people do not experience symptoms at all. Most people make a full recovery within a few weeks to several months. After this, they have immunity to it. Children under 6 years do not usually show any symptoms.
In rare cases, hepatitis A can be fatal. However, there are safe and effective vaccines that protect against this virus.
People at an increased risk for hepatitis A
1. international travelers
2. men who have sex with men
3. people with limited or no access to clean water
4. people living in areas with poor sanitation
5. sexual partners of people with hepatitis A
6. people experiencing homelessness
7. people who use recreational drugs and toxins
Diagnosis and treatment
Healthcare professionals typically make a hepatitis A diagnosis by performing blood tests. These tests can detect antibodies that are specific to hepatitis A.
There is no cure for hepatitis A, but treatment can help manage symptoms, and most people usually recover. The recovery process may take weeks or even months.
In rare cases, hepatitis A does not resolve, and people may experience complications such as acute liver failure. In such cases, liver transplantation may be lifesaving.
Hepatitis B
The CDC estimates that around 862,000 people in the U.S. are currently living with hepatitis B.
Infection with hepatitis B is usually acute or short term, but it can become chronic — especially in children.
Long-term complications, such as liver cancer or cirrhosis, can affect around 15–25% of people with chronic hepatitis B. There is no cure, but treatment can help manage the condition.
Hepatitis B typically spreads when the blood or semen of a person with the virus enters another person’s body.
Risk factors
1. having sexual intercourse without barrier methods
2. sharing needles
3. having a tattoo with unsterilized needles
4. sustaining accidental skin pricks with medical equipment
5. sharing personal items, such as a toothbrush or razor
6. breastfeeding by a person with the virus
7. birth by someone with the virus
Symptoms
ymptoms are similar to those of other types of hepatitis. People may initially be asymptomatic or may not display symptoms at all.
When a person with hepatitis B displays symptoms, they may include:
1. fever
2. skin rash
3. joint pain
4. arthritis
5. jaundice
6. fatigue
7. abdominal pain
8. nausea
9. anorexia
A safe and effective vaccine can protect people from hepatitis B infection. The number of cases has fallen dramatically in countries where the vaccine is available.
Diagnosis and treatment
Healthcare professionals will take several steps to diagnose hepatitis B. These include speaking with a person about sexual activity and needle use. The diagnostic process will also involve testing blood samples such as antibodies and antigens.
There is no cure for hepatitis B, which resolves on its own in 95% of cases. Supportive care can help manage symptoms. In cases of chronic illness, a doctor may prescribe an antiviral medication, and they will monitor the liver regularly to check for damage over time.
During treatment and recovery, a person should also avoid alcohol and drugs and supplements that are toxic to the liver.
Hepatitis B is the most common cause of chronic hepatitis and end-stage liver disease worldwide. Rarely, acute hepatitis B can lead to severe liver failure, which requires liver transplantation.
Hepatitis C
Hepatitis C is a blood-borne virus that usually transmits through people sharing needles or other drug-related equipment.
The CDC estimates that around 2.4 million people live with this virus in the U.S. The number has been growing since 2010.
Other people at risk of exposure include healthcare workers who handle sharps and children born to females with the virus.
It can be a short-term condition, but more than half of people with hepatitis C develop a chronic, long-term infection.
Symptoms
A person may have no symptoms, and around half of people living with the virus do not know they have it. They may transmit it to another person without realizing it.
When symptomatic, symptoms of hepatitis C typically include:
1. nausea
2. malaise
3. right upper quadrant pain
4. dark urine
5. jaundice
Diagnosis and treatment
As with hepatitis A and B, the primary diagnostic tool for hepatitis C is laboratory testing for hepatitis C antibodies.
According to the United Kingdom’s National Health Service (NHS), the body will eliminate the virus in around 25% of people. However, it can remain in the body and become chronic in others.
According to the CDC, there is no treatment for the acute stage of hepatitis C. If chronic hepatitis develops, they may prescribe a course of oral medication for 8–12 weeks, after which 9 out of 10 people will no longer have symptoms.
As with other types of hepatitis, people who have hepatitis C should avoid alcohol and drugs and supplements that are toxic to the liver.
In severe cases, Hepatitis C can cause liver scarring (cirrhosis), chronic liver disease and liver cancer. Hepatitis C-related complications are a leading cause of liver transplants in the U.S.
Hepatitis D
Hepatitis D is another viral hepatitis infection that can be acute and chronic. As with other hepatitis infections, it causes damage to a person’s liver.
However, these infections only occur in people who already have hepatitis B. The hepatitis D virus cannot establish itself otherwise. Around 5% of all people with a hepatitis B infection will develop a hepatitis D infection.
Symptoms
Most people with hepatitis D are asymptomatic.
When symptoms present, they are similar to those of other hepatitis infections. They include:
1. abdominal pain
2. nausea
3. vomiting
4. fever
5. jaundice
6. confusion
7. bruising
8. bleeding
Diagnosis and treatment
Doctors will make a hepatitis D diagnosis if they can find specific hepatitis D antibodies within a person’s bodily fluids. This process involves laboratory testing.
There is no known treatment for acute hepatitis D. Although some experimental work has shown that certain medications might help with chronic hepatitis D, the Food and Drug Administration (FDA) is yet to approve these treatments.
The hepatitis D infection can cause severe liver damage, and in some cases, a person may need a liver transplant.
Hepatitis E
Hepatitis E is a viral hepatitis infection that has acute and chronic forms. The chronic form is more common in immunosuppressed individuals.
The hepatitis E virus is the most frequent cause of acute hepatitis infections and causes over 50,000 deaths per year worldwide.
Symptoms
In many cases, hepatitis E infections are asymptomatic. When these infections are symptomatic, they tend to be fairly mild. Symptoms of hepatitis E include:
1. stomach pain
2. nausea
3. vomiting
4. jaundice
5. malaise
6. anorexia
Although a person can contract hepatitis E via blood transfusion, food or water that has come into contact with the feces of a person with the virus is the most common infection route.
Diagnosis and treatment
Healthcare professionals assess several different factors to make a hepatitis E diagnosis. These include their patient’s symptoms and travel history, as hepatitis E infections are endemic in some parts of the world.
Although scientists have not yet developed standardized tests for hepatitis E, laboratory testing is also important.
There is no standard line of treatment for hepatitis E infections, which usually resolve without treatment after a few weeks. However, in more serious and rare cases, a liver transplant may become necessary.
Prevention
The prevention of hepatitis transmission varies depending on the type.
Experts recommend regular screening for hepatitis A, B and C for those at higher risk. Doctors also routinely screen for hepatitis B and C during pregnancy.
The sections below discuss means of prevention by type.
Hepatitis A and E
Hepatitis A and E are most commonly spread through food and water that has come into contact with the feces of a person with the virus.
Some ways of preventing infection include:
1. washing the hands carefully after using the bathroom and before eating
2. ensuring that food is fully cooked and appropriately stored
3. drinking only bottled water when traveling
4. avoiding or peeling fruits and vegetables that may have been washed or grown in unsanitized water
People may ask their doctor about the hepatitis A vaccine, especially if they are traveling to an area where the virus is prevalent.
Hepatitis B, C, and D
To minimize the risk of transmission, where relevant, a person should:
1. talk openly with any sexual partners about any viruses they may have
2. use a barrier method, such as a condom, during sex
3. only use previously unused, clean needles
4. avoid sharing toothbrushes, razors, and manicure instruments
5. check that any tattoo or acupuncture equipment is sterile
People with a high risk of exposure to hepatitis B can ask their doctor about vaccination, but there is no vaccination for hepatitis C.
People who believe they may have hepatitis should seek medical help. A healthcare professional can advise on a person’s treatment, reduce the risk of complications and avoid transmitting the virus.
In people with HIV, there is a higher risk of contracting a hepatitis B or C infection. The impact can also be more severe, as the body is less able to fight the infection.
To lower their risk of hepatitis infection and complications, people with HIV should:
1. take precautions to prevent infection and transmission of hepatitis
2. attend all health checks
3. adhere to their treatment plan
Immunization can prevent hepatitis A and B, but not C. Treatment is available for hepatitis B and C, but not A.
Outlook
There are five hepatitis viruses, and each type has different characteristics. The outlook for people with hepatitis depends on the type, whether or not they have symptoms, and whether they seek treatment.
Some people do not know they have chronic hepatitis until liver failure occurs.
Different types of hepatitis have different chances of recovery. For example:
1. Hepatitis A:This type normally resolves within 2 months without having any long-term effects, and the person will have lifelong immunity afterward.
2. Hepatitis B:Most adults recover within 90 days and have lifelong immunity. However, according to the CDC, 90% of infants, 20–50% of older children aged 1–5 years, and 5% of adults develop a chronic infection. Chronic infection can lead to severe complications, such as liver cancer or cirrhosis.
3. Hepatitis C:The infection is chronic in 75–85% of people who have it, and 1–5% of people will experience life threatening complications. Treatment is available, but 15–25% of people will recover without it.
4. Hepatitis D:Although this infection is mostly benign in the long term, it only occurs in people with hepatitis B.
5. Hepatitis E:This infection often resolves on its own, without serious long-term harm. However, when someone has a rapidly worsening hepatitis E infection, the fatality rate will be between 0.5–3%.
People who suspect they have hepatitis should speak with a healthcare professional as soon as possible.
Frequently Asked Questions About Viral Hepatitis
Sometimes after overcoming an acute hepatitis B infection, something causes your immune system to weaken against the virus later in life. Maybe your immune system was strong at the time of infection, but now you have a condition that weakens it.
When this happens, the once-defeated virus can become active in your body again. Reactivated hepatitis B can be temporary or lasting. But because it tends to occur in immune-suppressed people, it may be especially severe and even cause acute liver failure.
You’re contagious as long as the virus is active in your body. If you have an acute infection, it may last from a few weeks to six months, and you’re contagious that whole time. If you have a chronic infection, you’re contagious as long as it lasts, which is usually for life.
A healthcare provider may offer you different treatment options based on the type of the hepatitis and status of the infection.
If you only have a temporary, acute infection, chances are good your immune system will overcome it shortly. Once you’ve recovered from an acute infection, you won’t get it again. A blood test can tell you if you’ve overcome the virus and become immune.
If you don’t overcome it during the acute phase of infection, you’ll develop a chronic infection, which is lifelong. Chronic hepatitis B isn’t curable, but it’s manageable with treatment. A blood test can tell you if you need treatment for a chronic infection.