An overview of Acute Kidney Disease
What is Acute kidney injury?
Acute Kidney Injury (AKI), formerly known as acute renal failure, is a sudden and rapid decline in kidney function that occurs over a short period of time, ranging from hours to a few days. AKI can be a serious medical condition that requires prompt diagnosis and treatment, as it can lead to various complications and affect multiple organ systems.
AKI is characterized by a sudden decrease in the kidneys' ability to filter waste products and excess fluids from the blood, resulting in the accumulation of waste and electrolyte imbalances.
Types of Acute kidney injury
Acute Kidney Injury (AKI), also known as acute renal failure, can be classified into three main types based on the underlying causes and mechanisms that lead to the sudden decline in kidney function. These types help guide diagnosis and treatment. The three types of AKI are:
1. Prerenal AKI: This type of AKI occurs when there is a decrease in blood flow to the kidneys, leading to inadequate filtration and subsequent kidney dysfunction. The reduced blood flow can be caused by conditions that affect the circulation or volume of blood before it reaches the kidneys. Common causes of prerenal AKI include:
Dehydration
Reduced blood volume due to bleeding or fluid loss
Severe infections or sepsis
Heart failure or cardiac issues that compromise blood flow
Medications that affect blood pressure or blood flow
2. Intrinsic (Intrarenal) AKI: Intrinsic AKI involves damage to the kidney tissue itself, affecting the structures within the kidneys responsible for filtration and urine production. This type of AKI can result from various conditions that directly impact the kidney's functioning. Common causes of intrinsic AKI include:
Acute Tubular Necrosis (ATN): This is a condition where the kidney tubules, responsible for filtering and reabsorbing substances from the blood, become damaged. ATN can be caused by factors such as ischemia (lack of blood flow) or exposure to nephrotoxic substances like certain medications or contrast agents.
Glomerulonephritis: Inflammation of the glomeruli, the tiny filtering units in the kidneys, can lead to AKI. This can be caused by autoimmune diseases, infections, or other factors.
Acute Interstitial Nephritis: Inflammation of the kidney's interstitial tissue, often caused by allergic reactions to medications or infections, can result in AKI.
Acute Vascular Injury: Conditions that affect the blood vessels within the kidneys, such as vasculitis or thrombotic microangiopathies, can lead to AKI.
3. Postrenal AKI: Postrenal AKI occurs due to an obstruction that prevents the flow of urine out of the kidneys. This obstruction can lead to a buildup of pressure in the kidneys, causing kidney dysfunction. Common causes of postrenal AKI include:
Kidney stones
Urinary tract obstructions
Enlarged prostate gland (in males)
Tumors that block urine flow
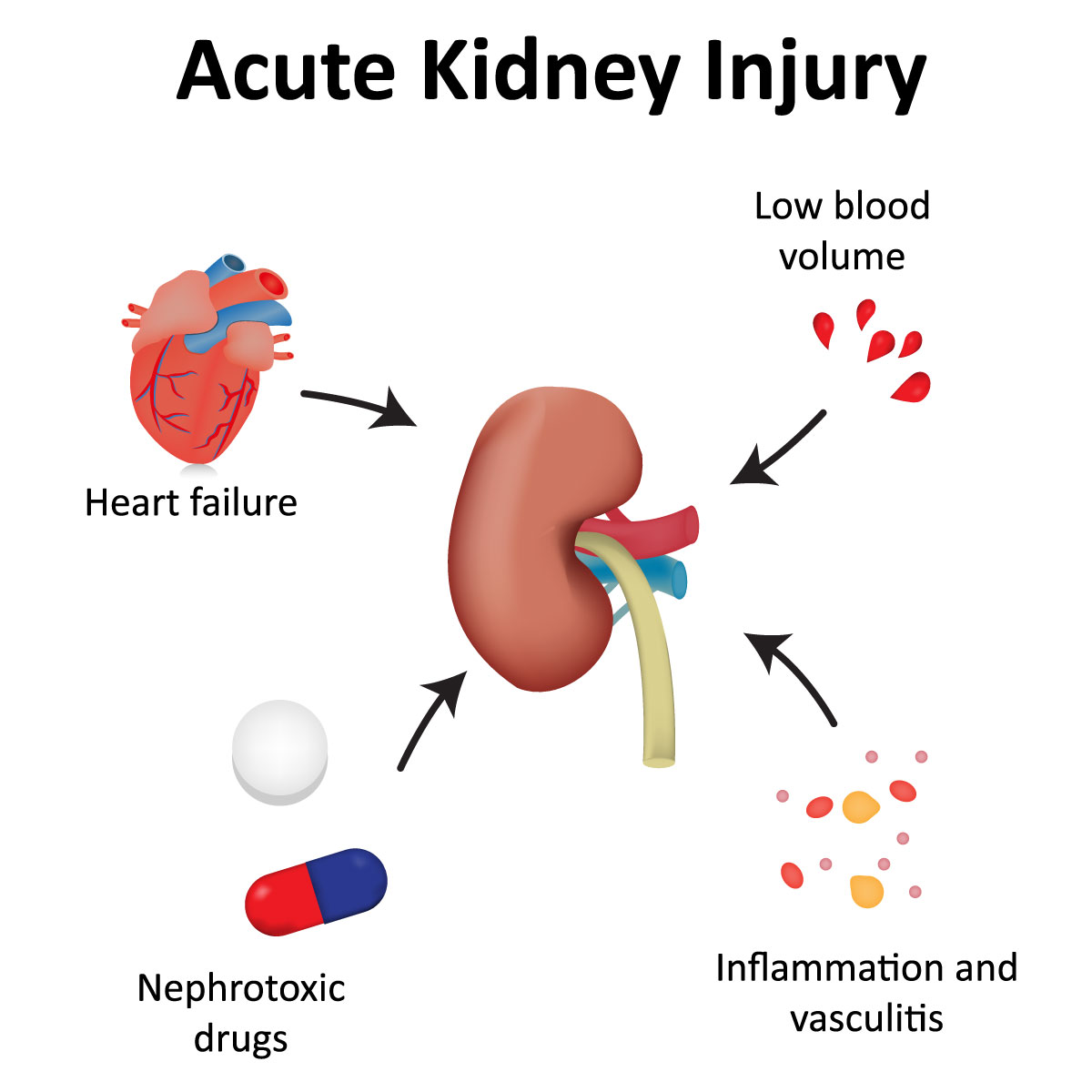
Causes of Acute kidney injury
There are various potential causes of AKI, which can be broadly categorized into three main groups: prerenal, intrinsic renal, and postrenal causes.
1. Prerenal Causes: Prerenal causes of AKI occur when there is a decreased blood flow to the kidneys, leading to inadequate perfusion and oxygen delivery. Common prerenal causes include:
Hypovolemia: Decreased blood volume due to dehydration, blood loss, or excessive fluid loss.
Hypotension: Low blood pressure, which can be caused by various factors, including severe infections, heart failure, or shock.
EReduced Cardiac Output: Conditions like heart failure, cardiac arrhythmias, and myocardial infarction can lead to reduced blood flow to the kidneys.
Vasoconstriction: Conditions that cause blood vessels to constrict, such as sepsis or certain medications, can reduce blood flow to the kidneys.
2. Intrinsic Renal Causes: Intrinsic renal causes of AKI involve damage to the kidney tissues themselves. These causes can result in direct damage to the renal cells and structures, leading to impaired kidney function. Common intrinsic renal causes include:
Acute Tubular Necrosis (ATN): Damage to the tubular cells of the kidneys due to ischemia (lack of blood flow) or exposure to nephrotoxic substances, such as certain medications or contrast agents.
Glomerulonephritis: Inflammation of the glomeruli (filtering units) of the kidneys, often caused by autoimmune reactions or infections.
Interstitial Nephritis: Inflammation of the interstitial tissue between the tubules, often caused by allergic reactions to medications or infections.
Acute Interstitial Nephritis: Inflammation of the interstitial tissue between the tubules, often caused by allergic reactions to medications or infections.
Vascular Diseases: Conditions affecting the blood vessels in the kidneys, such as vasculitis or thrombotic microangiopathies.
3. Postrenal Causes: Postrenal causes of AKI occur when there is obstruction of urine flow from the kidneys, leading to back pressure and damage. Common postrenal causes include:
Urinary Tract Obstruction: Blockages in the urinary tract, such as kidney stones, tumors, or enlarged prostate glands, can lead to AKI.
Bladder Outlet Obstruction: Blockages at the bladder outlet, such as urethral strictures, can prevent proper urine flow.
Ureteral Obstruction: Blockages in the ureters, which are the tubes connecting the kidneys to the bladder, can result in backflow of urine.
Signs and symptoms of Acute kidney injury
The symptoms of AKI can vary in severity depending on the underlying cause and the extent of kidney damage. These symptoms can be nonspecific and may overlap with other medical conditions. Common signs and symptoms of acute kidney injury include:
1. Decreased Urine Output: One of the hallmark signs of AKI is a decrease in urine output, known as oliguria. In some cases, urine output may be almost nonexistent. This occurs because the kidneys are unable to effectively filter and excrete waste products and fluids.
2. Fluid Retention and Edema: Fluid that is not being excreted through urine can lead to fluid retention, causing swelling in the ankles, legs, and even the face. This condition is known as edema.
3. Fatigue and Weakness: The accumulation of waste products and toxins in the blood due to reduced kidney function can lead to feelings of fatigue, weakness, and overall malaise.
4.Shortness of Breath: Excess fluid in the body can also accumulate in the lungs, leading to difficulty breathing and shortness of breath.
5. Confusion and Altered Mental Status: The accumulation of waste products and electrolyte imbalances can affect brain function, causing confusion, disorientation, and even delirium.
6. Nausea and Vomiting: The build-up of waste products in the blood can lead to nausea and vomiting.
7. Decreased Appetite and Weight Loss
8. Irregular Heartbeat and Chest Pain
9. Muscle Weakness and Cramps
10. High Blood Pressure (Hypertension)
11. Back Pain or Flank Pain
12. Seizures or Coma (in severe cases)
Preventive measures against Acute kidney injury
Preventing acute kidney injury (AKI) involves avoiding situations and behaviors that can contribute to kidney damage, as well as addressing underlying health conditions that might increase your risk. Here are some preventive measures you can take:
1. Hydration: Stay well-hydrated, especially during hot weather, exercise, or when you're ill. Proper hydration helps maintain blood flow to the kidneys and supports their normal function.
2. Medication Safety: Be cautious with over-the-counter pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen. These medications can cause kidney damage, especially when taken in excess or for extended periods. Always follow dosing instructions and consult your healthcare provider if you have concerns.
3. Avoid Nephrotoxic Substances: Be aware of substances that can harm the kidneys. These may include certain medications (like antibiotics or antifungal agents), herbal supplements, recreational drugs, and exposure to chemicals or toxins.
4. Manage Underlying Health Conditions: Properly manage health conditions that can contribute to AKI, such as diabetes, high blood pressure, and heart conditions. Regular check-ups, medication adherence, and lifestyle modifications are key.
5. Avoid Dehydration
6. Properly Manage Kidney Stones: If you have a history of kidney stones, work with your healthcare provider to manage and prevent future episodes. Adequate hydration and dietary modifications may be recommended.
7. Use Contrast Agents with Caution: If you're undergoing medical procedures that require the use of contrast agents (e.g., for imaging studies), discuss any pre-existing kidney conditions with your healthcare provider. They can help determine the safest approach.
8. Prevent Infections: Prevent urinary tract infections (UTIs) and other infections, especially if you have underlying conditions that increase your susceptibility. Maintain good hygiene and seek prompt medical treatment if you suspect an infection.
9. Avoid Excessive Alcohol Consumption
10. Balanced Diet and Regular Exercise: Adopt a healthy lifestyle with a balanced diet and regular physical activity to maintain overall health and support proper kidney function.
11. Seek Prompt Medical Attention
Remember that early detection and management of underlying conditions are key to preventing complications like ACKD. If you have concerns about your kidney health or risk factors, consult your healthcare provider for personalized advice and guidance.
12. Know Your Medications: Inform your healthcare provider about all the medications you're taking, including prescription, over-the-counter, and herbal supplements. This information helps them assess potential risks and interactions.
How Is Acute kidney injury Diagnosed?
Acute kidney injury (AKI) is diagnosed through a combination of clinical assessment, medical history, laboratory tests, and imaging studies. Prompt and accurate diagnosis is essential for determining the cause of AKI and guiding appropriate treatment. Here's how the diagnosis process typically works:
1. Medical History and Physical Examination: Your healthcare provider will ask about your medical history, recent illnesses, medications you're taking, and any other factors that might contribute to kidney damage. They will also perform a physical examination to assess signs of fluid retention, dehydration, or other symptoms related to AKI.
2. Laboratory Tests: Blood and urine tests play a crucial role in diagnosing AKI and determining its severity. Common tests include:
Serum Creatinine: Elevated levels of creatinine in the blood indicate reduced kidney function. Changes in creatinine levels over time can help assess the severity and progression of AKI.
Blood Urea Nitrogen (BUN): Elevated BUN levels can indicate impaired kidney function.
Urine Tests: Urine tests help assess kidney function and identify factors contributing to AKI. These include the urinalysis and measurements of urine output.
Electrolyte Levels: Imbalances in electrolytes like sodium, potassium, and calcium are common in AKI and need to be monitored closely.
3. Imaging Studies: Imaging tests such as ultrasound, CT scans, or MRI may be conducted to visualize the kidneys and identify any structural abnormalities, obstructions, or signs of damage.
4. Urine Output Monitoring: Monitoring your urine output is essential in assessing kidney function. A decrease in urine output may indicate AKI.
5. Medical History Review: Reviewing your medical history can help identify risk factors for AKI, such as recent surgeries, medication use, infections, or exposure to nephrotoxic substances.
6. Classification of AKI Severity: AKI severity is classified into stages based on serum creatinine levels and urine output. This classification helps guide treatment decisions and prognosis.
7. Underlying Causes Assessment: Identifying the underlying cause of AKI is crucial. It may be due to prerenal causes (e.g., low blood flow to the kidneys), intrinsic renal causes (e.g., acute tubular necrosis), or postrenal causes (e.g., urinary tract obstruction). Your medical history and test results will help pinpoint the cause.
8. Continuous Monitoring:Continuous monitoring of your clinical status, kidney function, electrolyte levels, and fluid balance is essential during the diagnostic and treatment phases.
AKI is a serious condition that requires timely diagnosis and intervention. If you suspect you have symptoms of AKI, such as decreased urine output, swelling, or changes in mental status, seek medical attention promptly. Early diagnosis and management can help prevent further kidney damage and improve outcomes.
Treatment for Acute kidney injury
The treatment for acute kidney injury (AKI) involves addressing the underlying cause of the condition, managing symptoms, and providing supportive care to help the kidneys recover. AKI is a sudden and often reversible decrease in kidney function that can occur due to various factors such as dehydration, infections, medications, and more. Here are the general steps in treating AKI:
1. Identify and Address Underlying Causes:The first step is to identify and treat the underlying cause of AKI. This could involve discontinuing medications that might be contributing to the problem, treating infections, managing fluid and electrolyte imbalances, and addressing conditions like kidney stones or obstruction.
2.Fluid Management:In cases of AKI, there can be fluid imbalances in the body. Depending on the cause and severity of AKI, healthcare providers may need to adjust fluid intake and output to prevent dehydration or fluid overload. Intravenous (IV) fluids might be administered to maintain appropriate hydration levels.
3. Medication Review:Some medications can be harmful to the kidneys or might need dosage adjustments in individuals with AKI. Healthcare providers will review the individual's medication list and make necessary changes to avoid further kidney damage.
4. Electrolyte Management:AKI can lead to imbalances in electrolytes such as potassium, sodium, and calcium. Monitoring and correcting these imbalances are essential for overall health.
5.Nutritional Support:A balanced diet that takes into consideration the individual's kidney function is important during AKI. Depending on the severity of AKI, adjustments in protein, sodium, and potassium intake might be necessary.
6. Monitoring and Follow-up:Regular monitoring of kidney function, electrolyte levels, and overall health is crucial during the recovery phase. This might involve blood tests and other diagnostic measures.
7. Dialysis:In severe cases of AKI where the kidneys are not able to adequately filter waste and excess fluids from the blood, dialysis might be necessary. Dialysis is a medical procedure that helps remove waste and excess fluids from the body.
8. Treatment of Complications:AKI can lead to various complications, including cardiovascular issues and fluid overload. These complications may need additional treatments and management.
9. Preventing Future Episodes:Depending on the cause of AKI, steps might need to be taken to prevent its recurrence. This could involve avoiding nephrotoxic medications, managing chronic conditions like diabetes or hypertension, and maintaining a healthy lifestyle.
Treatment for AKI is highly individualized based on the cause, severity, and the patient's overall health status. It's important to work closely with healthcare professionals, including nephrologists and other specialists, to develop a tailored treatment plan and achieve the best possible outcomes.
What are the Acute kidney injury stages?
AKI is typically classified into stages based on the severity of the impairment, using criteria such as serum creatinine levels and urine output. The most commonly used classification system for AKI stages is the Kidney Disease: Improving Global Outcomes (KDIGO) criteria. The KDIGO AKI staging system consists of three stages:
1. Stage 1 AKI:
2. Stage 2 AKI::
1. Stage 3 AKI:
Frequently Asked Questions About Acute kidney injury
A: Common causes of AKI include severe infections, dehydration, certain medications (like NSAIDs and certain antibiotics), kidney diseases, and reduced blood flow to the kidneys (e.g., due to low blood pressure or surgery).
A: Symptoms of AKI can include decreased urine output, swelling, fatigue, confusion, nausea, and vomiting. In severe cases, it may lead to seizures or coma.
A: In many cases, AKI is reversible, especially if detected and treated early. However, if the kidney damage is severe or if the underlying cause is not addressed, it can lead to chronic kidney disease (CKD).
A: No, AKI and CKD are different conditions. AKI is a sudden decline in kidney function, whereas CKD is a long-term, progressive loss of kidney function. However, severe or recurrent AKI can increase the risk of developing CKD.