An overview of Diabetic Kidney Disease
What is Diabetic kidney Disease?
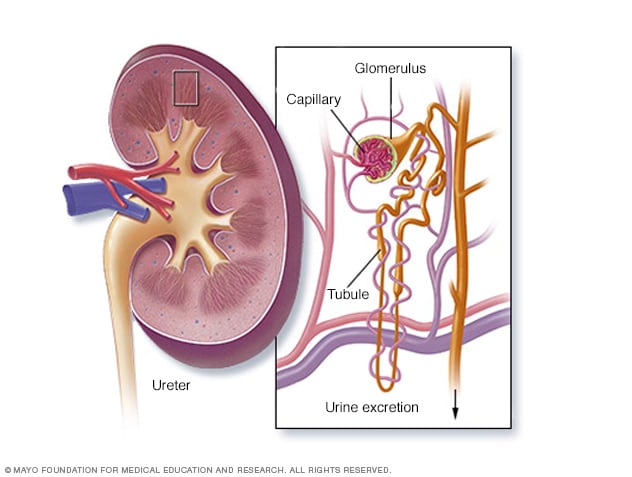
Diabetic kidney disease, also known as diabetic nephropathy, is a complication of diabetes that affects the kidneys. It is a leading cause of chronic kidney disease (CKD) and end-stage renal disease (ESRD) worldwide. Diabetic kidney disease develops over time due to the long-term impact of high blood sugar levels on the blood vessels and filtering units (glomeruli) in the kidneys.
Diabetes, particularly type 1 and type 2 diabetes, can lead to damage in the small blood vessels throughout the body, including those in the kidneys. This damage, combined with other factors like high blood pressure, inflammation, and genetic predisposition, can result in diabetic kidney disease.
Your kidneys contain millions of tiny blood vessel clusters (glomeruli) that filter waste from your blood. Severe damage to these blood vessels can lead to diabetic nephropathy, decreased kidney function and kidney failure.
Types of Diabetic kidney Disease
Diabetic kidney disease, also known as diabetic nephropathy, can be categorized into different types based on its clinical presentation and underlying characteristics. Here are a few types of diabetic kidney disease that are commonly recognized:
1. Classic Diabetic Nephropathy: This is the most common type of diabetic kidney disease and occurs in individuals with both type 1 and type 2 diabetes. It typically follows a predictable progression from the initial stages of hyperfiltration and microalbuminuria to significant proteinuria and reduced kidney function. Classic diabetic nephropathy is characterized by the deposition of excess matrix material within the glomeruli of the kidneys, leading to scarring and loss of function.
2. Non-albuminuric Diabetic Kidney Disease: While albuminuria (presence of albumin in the urine) is a hallmark of diabetic kidney disease, some individuals with diabetes may experience kidney damage without significant albuminuria. This form of diabetic kidney disease is called non-albuminuric diabetic kidney disease. It suggests that kidney damage can occur even in the absence of detectable proteinuria.
3. Rapid Progression Diabetic Nephropathy: In some cases, diabetic kidney disease may progress more rapidly than usual, leading to significant kidney damage and dysfunction over a shorter period. This can result in a quicker decline in kidney function and an increased risk of reaching end-stage renal disease (ESRD) sooner.
4. Renal Insufficiency Diabetic Nephropathy: This type of diabetic kidney disease is characterized by significant renal insufficiency, which means the kidneys are not able to perform their filtration and waste removal functions adequately. Individuals with this type of nephropathy may experience substantial reductions in glomerular filtration rate (GFR) and may require kidney replacement therapies like dialysis or transplantation.
5. Arterionephrosclerosis: In some cases, diabetes can lead to widespread damage to the blood vessels, including those in the kidneys. This can result in arterionephrosclerosis, a condition where the blood vessels in the kidneys become thickened and narrowed. The reduced blood flow to the kidneys can contribute to kidney damage and dysfunction.
Causes of Diabetic kidney Disease
Diabetic kidney disease, also known as diabetic nephropathy, is a common complication of diabetes mellitus. It occurs when prolonged high blood sugar levels damage the small blood vessels in the kidneys, leading to impaired kidney function over time. Several factors contribute to the development and progression of diabetic kidney disease:
1. Hyperglycemia:: Prolonged high levels of glucose in the blood, known as hyperglycemia, are the primary trigger for diabetic kidney disease. Elevated glucose levels cause damage to the blood vessels, including those in the kidneys, impairing their ability to filter waste products from the blood effectively.
2. Hypertension (High Blood Pressure): Diabetes often leads to high blood pressure, which can further damage the blood vessels and structures in the kidneys. Hypertension increases the stress on the already compromised blood vessels, accelerating kidney damage.
3.Genetic Factors: Genetic predisposition can play a role in an individual's susceptibility to diabetic kidney disease. Some people may be more genetically prone to developing kidney complications as a result of diabetes.
4. Duration of Diabetes: The longer an individual has diabetes, the higher their risk of developing diabetic kidney disease. This is why managing diabetes from an early stage is crucial in preventing or delaying the onset of complications.
5. Poor Blood Sugar Control: Inadequate management of blood sugar levels, including frequent fluctuations, can contribute to kidney damage. Tight glycemic control through proper diet, exercise, and medications can help mitigate this risk.
6. Obesity: Excess body weight, especially abdominal obesity, is associated with an increased risk of diabetic kidney disease. Obesity can lead to insulin resistance and other metabolic abnormalities that contribute to kidney damage.
7. Dyslipidemia: Abnormal levels of lipids (cholesterol and triglycerides) in the blood can worsen kidney disease in people with diabetes. Elevated lipids contribute to the development of atherosclerosis, which affects the blood vessels supplying the kidneys.
8. Smoking: Smoking is a risk factor for many health problems, including diabetic kidney disease. It exacerbates the damage to blood vessels, including those in the kidneys.
9. Albuminuria: The presence of excess protein (albumin) in the urine, known as albuminuria or proteinuria, is an early sign of kidney damage. It indicates that the filtering function of the kidneys is impaired.
10. Inflammation: Chronic low-level inflammation, common in diabetes, can contribute to kidney damage. Inflammatory processes can worsen blood vessel health and promote tissue damage in the kidneys.
11. Gender and Age: Men with diabetes are generally at a higher risk of developing kidney disease compared to women with diabetes. Additionally, the risk of kidney disease increases with age.
It's important for individuals with diabetes to manage their condition effectively through a combination of maintaining healthy blood sugar levels, controlling blood pressure, adopting a balanced diet, engaging in regular physical activity, not smoking, and following medical advice to prevent or delay the onset of diabetic kidney disease. Regular check-ups and early intervention are crucial for monitoring kidney function and managing any complications that may arise.
Signs and symptoms of Diabetic kidney Disease
Diabetic kidney disease, also known as diabetic nephropathy, often develops over a period of years and may not exhibit noticeable symptoms in its early stages. However, as the condition progresses, certain signs and symptoms can arise. It's important to note that these symptoms may not be specific to diabetic kidney disease alone and could overlap with other conditions, so proper medical evaluation is essential for accurate diagnosis. Common signs and symptoms of diabetic kidney disease include:
1.Proteinuria (Presence of Protein in Urine): Excessive amounts of protein, specifically albumin, in the urine (albuminuria) is an early sign of kidney damage. It can be detected through urine tests and is often one of the first indications of diabetic kidney disease.
2. Swelling (Edema): Fluid retention can lead to swelling, particularly in the ankles, feet, legs, and around the eyes. This occurs because the kidneys are less able to remove excess fluid and sodium from the body.
3. High Blood Pressure (Hypertension): Diabetic kidney disease can lead to increased blood pressure. Conversely, high blood pressure can also contribute to the development and progression of kidney disease. Elevated blood pressure can further damage the blood vessels in the kidneys.
4.Fatigue and Weakness: As kidney function declines, waste products and toxins can build up in the blood, leading to a feeling of fatigue and overall weakness.
5. Increased Urination (Polyuria):The kidneys' ability to concentrate urine decreases as kidney function worsens. This can lead to increased frequency of urination, especially at night (nocturia).
6. Puffiness Around the Eyes: Swelling or puffiness, particularly around the eyes, can be a visible sign of fluid retention.
7. Decreased Appetite and Weight Loss: Reduced kidney function can cause loss of appetite and unintentional weight loss.
8. Nausea and Vomiting: Accumulation of waste products in the blood can lead to nausea and vomiting.
9. Itchy Skin
10. Muscle Cramps
11. Changes in Urine Color and Foaminess
12. Back Pain or Flank Pain
It's important to note that these symptoms can vary in intensity and may not necessarily appear in every individual with diabetic kidney disease. Regular monitoring of kidney function through blood tests and urine tests is essential for early detection and management of diabetic kidney disease. If you have diabetes, it's crucial to work closely with your healthcare provider to manage your condition and undergo regular check-ups to monitor your kidney health.
Preventive measures against Diabetic kidney Disease
Preventing diabetic kidney disease involves managing your diabetes effectively and adopting a healthy lifestyle. Here are some key preventive measures you can take:
1. Manage Blood Sugar Levels: Keeping your blood sugar levels within a target range is crucial. Consistently high blood sugar levels can damage blood vessels, including those in the kidneys. Follow your healthcare provider's recommendations for monitoring and controlling your blood sugar through diet, exercise, and medications if necessary.
2. Control Blood Pressure: High blood pressure (hypertension) is a significant risk factor for diabetic kidney disease. Work with your healthcare provider to maintain a healthy blood pressure level. Lifestyle changes, such as reducing salt intake, exercising regularly, and taking prescribed medications, can help manage blood pressure.
3. Adopt a Healthy Diet: Focus on a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit your intake of processed foods, sugary beverages, and foods high in saturated and trans fats. Controlling your carbohydrate intake and choosing foods with a low glycemic index can also help manage blood sugar levels.
4. Regular Physical Activity:Engage in regular exercise to help control your weight, improve insulin sensitivity, and promote cardiovascular health. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, along with strength training.
5. Quit Smoking: Smoking is harmful to your overall health and can worsen kidney damage. If you smoke, seek support to quit smoking. Your healthcare provider can provide resources and strategies to help you quit.
6. Limit Alcohol Consumption: If you choose to drink alcohol, do so in moderation. Excessive alcohol consumption can contribute to high blood pressure and negatively affect kidney health.
7. Maintain a Healthy Weight: Maintaining a healthy weight through a combination of balanced eating and regular physical activity can help reduce your risk of both diabetes and diabetic kidney disease.
8. Monitor Kidney Function: Regularly monitor your kidney function through urine and blood tests, especially if you have diabetes. Early detection of kidney damage can help you and your healthcare provider take appropriate measures to manage and slow the progression of the disease.
9. Take Medications as Prescribed
10. Stay Hydrated
Regular Medical Check-ups
How Is Diabetic kidney Disease Diagnosed?
Diabetic kidney disease is diagnosed through a combination of medical history, physical examination, and various tests that assess kidney function and detect signs of kidney damage. If you have diabetes or are at risk of developing diabetic kidney disease, your healthcare provider will monitor your kidney health regularly. Here's how the diagnosis process typically works:
1. Medical History and Physical Examination: Your healthcare provider will inquire about your medical history, including any history of diabetes, blood pressure issues, and kidney disease in your family. They will also conduct a physical examination to assess your overall health and check for signs of kidney disease, such as swelling and high blood pressure.
2. Urine Tests: Urine tests are commonly used to detect early signs of kidney damage. Two key tests are:
Albumin-to-Creatinine Ratio (ACR):This test measures the amount of albumin (a protein) in your urine compared to the level of creatinine. Increased levels of albumin in the urine (albuminuria) can be an early sign of kidney damage.
Estimated Glomerular Filtration Rate (eGFR): This test estimates how well your kidneys are filtering waste from your blood. A decreased eGFR indicates reduced kidney function.
3. Blood Tests.
4. Kidney Imaging.
5. Kidney Biopsy (If Necessary).
6. Regular Monitoring.
Treatment for Diabetic kidney Disease
Managing DKD involves a combination of lifestyle changes, medications, and close medical supervision. Here are some common approaches to treating DKD:
1. Blood Sugar Control (Glycemic Control):Maintaining good control of blood sugar levels is crucial in slowing the progression of DKD. This typically involves monitoring blood glucose regularly, adhering to a balanced diet, and taking medications as prescribed by a healthcare provider.
2.Blood Pressure Management:High blood pressure can exacerbate kidney damage in individuals with DKD. Doctors often recommend maintaining blood pressure at or below specific targets. Lifestyle changes, such as reducing sodium intake, regular exercise, and medications (like angiotensin-converting enzyme inhibitors or angiotensin receptor blockers), may be prescribed to manage blood pressure effectively.
3. Medications:In addition to blood pressure medications, doctors might prescribe medications to help manage other factors contributing to DKD progression, such as high cholesterol (statins) and anemia.
4. Dietary Modifications:A dietitian can create a personalized eating plan that helps manage blood sugar levels, blood pressure, and overall kidney health. A balanced diet that limits sodium, potassium, and phosphorus can be important.
5.Exercise:Regular physical activity can improve insulin sensitivity, help manage blood sugar levels, and promote overall cardiovascular health.
6. Smoking Cessation:If the individual smokes, quitting smoking is highly recommended, as smoking can worsen kidney function and increase the risk of cardiovascular complications.
7. Weight Management:Maintaining a healthy weight is important for overall health and can have a positive impact on diabetes and kidney function.
8. Regular Monitoring:Individuals with DKD should have regular check-ups with healthcare providers to monitor kidney function, blood sugar levels, blood pressure, and other relevant markers.
9. Advanced Treatments:In cases where DKD has progressed to more advanced stages, treatments such as dialysis or kidney transplantation might be considered. These options are usually explored in collaboration with nephrologists and transplant specialists.
What are the Diabetic kidney Disease stages?
Diabetic kidney disease progresses through several stages. These stages are determined based on the extent of kidney damage and the level of kidney function. The stages are often classified using a system called the "stages of chronic kidney disease" (CKD), which includes stages 1 through 5. Here are the stages of diabetic kidney disease:
1.Stage 1 CKD: In this stage, kidney damage is present, but kidney function (measured by glomerular filtration rate or GFR) is normal or only slightly reduced. Urine tests may show the presence of small amounts of albumin (a protein) in the urine, which is an early sign of kidney damage.
2.Stage 2 CKD: Kidney damage is more pronounced, and there may be mild to moderate reductions in kidney function. Albuminuria (the presence of more significant amounts of albumin in the urine) may become more evident.
3.Stage 3 CKD: At this stage, kidney function is moderately reduced. It is further divided into two sub-stages:
Stage 3a: Kidney function is moderately reduced, with a GFR between 45 and 59 mL/min.
Stage 3b: Kidney function is moderately reduced, with a GFR between 30 and 44 mL/min.
4.Stage 4 CKD: Kidney function is severely reduced, with a GFR between 15 and 29 mL/min. This stage often requires advanced medical management, including discussions about kidney replacement therapy such as dialysis or kidney transplantation.
5.Stage 5 CKD: This is also known as end-stage renal disease (ESRD). Kidney function is very severely reduced, with a GFR less than 15 mL/min. At this point, most individuals with ESRD require kidney replacement therapy, such as dialysis or a kidney transplant, to survive.
Frequently Asked Questions About Diabetic kidney Disease
A: Diabetic kidney disease, or DKD, is a type of kidney disease that occurs as a complication of diabetes. It is characterized by damage to the kidneys caused by high blood sugar levels over an extended period.
A: The primary cause of diabetic kidney disease is uncontrolled or poorly controlled diabetes, especially over a long time. Both type 1 and type 2 diabetes can lead to DKD.
A: In its early stages, DKD may not cause noticeable symptoms. As it progresses, symptoms may include swelling (edema), increased protein in the urine, high blood pressure, fatigue, and changes in urination patterns.
A: DKD is diagnosed through blood and urine tests. Blood tests measure kidney function (glomerular filtration rate or GFR), and urine tests check for the presence of albumin (a protein) in the urine.