An overview of Osteoporosis
What is Osteoporosis?
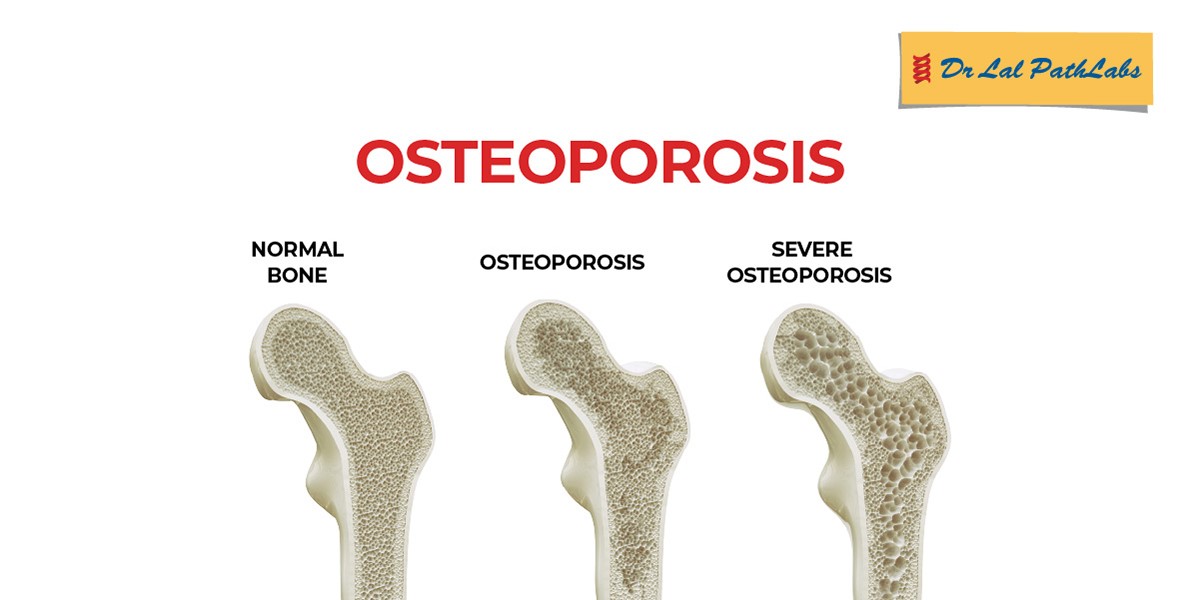
Osteoporosis is a disease that weakens your bones. It makes your bones thinner and less dense than they should be. People with osteoporosis are much more likely to experience broken bones (bone fractures).
Your bones are usually dense and strong enough to support your weight and absorb most kinds of impacts. As you age, your bones naturally lose some of their density and their ability to regrow (remodel) themselves. If you have osteoporosis your bones are much more fragile than they should be, and are much weaker.
Most people don’t know they have osteoporosis until it causes them to break a bone. Osteoporosis can make any of your bones more likely to break, but the most commonly affected bones include your:
1. Hips (hip fractures).
2. Wrists.
3. Spine (fractured vertebrae).
The sooner a healthcare provider diagnoses osteoporosis, the less likely you are to experience bone fractures. Ask a healthcare provider about checking your bone density, especially if you’re over 65, have had a bone fracture after age 50, or someone in your biological family has osteoporosis.
Osteoporosis risk factors
Anyone can develop osteoporosis. Some groups of people are more likely to experience it, including:
1. Anyone over 50.
2. People assigned female at birth (AFAB), especially people AFAB in postmenopause.
3. People with a family history (if someone in your biological family has osteoporosis).
4. People who are naturally thin or who have “smaller frames.” People with thinner statures often have less natural bone mass, so any losses can affect them more.
5. People who smoke or use tobacco products.
Some health conditions can make you more likely to develop osteoporosis, including:
1. Endocrine disorders — any condition that affects your parathyroid glands, thyroid gland and hormones (like thyroid disease and diabetes).
2. Gastrointestinal diseases (like celiac disease and inflammatory bowel disease [IBD]).
3. Autoimmune disorders that affect your bones (like rheumatoid arthritis or ankylosing spondylitis — arthritis that affects your spine).
4. Blood disorders (or cancers that affect your blood like multiple myeloma).
Some medications or surgical procedures can increase your risk of osteoporosis:
1. Diuretics (medications that lower your blood pressure and clear extra fluid from your body).
2. Corticosteroids (medications that treat inflammation).
3. Medications used to treat seizures.
4. Bariatric (weight loss) surgery.
5. Hormone therapy for cancer (including to treat breast cancer or prostate cancer).
6. Anticoagulants.
7. Proton pump inhibitors (like those that treat acid reflux, which can affect your calcium absorption).
Certain aspects of your diet and exercise routine can make you more likely to develop osteoporosis, including:
1. Not getting enough calcium or vitamin D in your diet.
2. Not getting enough physical exercise.
3. Regularly drinking alcohol (more than two drinks per day).
Causes of Osteoporosis
Osteoporosis happens as you get older and your bones lose their ability to regrow and reform themselves
Your bones are living tissue like any other part of your body. It might not seem like it, but they’re constantly replacing their own cells and tissue throughout your life. Up until about age 30, your body naturally builds more bone than you lose. After age 35, bone breakdown happens faster than your body can replace it, which causes a gradual loss of bone mass.
If you have osteoporosis, you lose bone mass at a greater rate. People in postmenopause lose bone mass even faster.
Signs and symptoms of Osteoporosis
Osteoporosis doesn’t have symptoms the way lots of other health conditions do. That’s why healthcare providers sometimes call it a silent disease.
You won’t feel or notice anything that signals you might have osteoporosis. You won’t have a headache, fever or stomachache that lets you know something in your body is wrong.
The most common “symptom” is suddenly breaking a bone, especially after a small fall or minor accident that usually wouldn’t hurt you.
Even though osteoporosis doesn’t directly cause symptoms, you might notice a few changes in your body that can mean your bones are losing strength or density. These warning signs of osteoporosis can include:
1. Losing an inch or more of your height.
2. Changes in your natural posture (stooping or bending forward more).
3. Shortness of breath (if disks in your spine are compressed enough to reduce your lung capacity).
4. Lower back pain (pain in your lumbar spine).
It might be hard to notice changes in your own physical appearance. A loved one may be more likely to see changes in your body (especially your height or posture). People sometimes joke about older adults “shrinking” as they age, but this can be a sign that you should visit a healthcare provider for a bone density test.
Preventive measures against Osteoporosis
Exercise and making sure you get enough calcium and vitamin D in your diet are usually all you’ll need to prevent osteoporosis. Your provider will help you find a combination of treatments that’s best for you and your bone health.
Follow these general safety tips to reduce your risk of an injury:
1. Always wear your seatbelt.
2. Wear the right protective equipment for all activities and sports.
3. Make sure your home and workspace are free from clutter that could trip you or others.
4. Always use the proper tools or equipment at home to reach things. Never stand on chairs, tables or countertops.
5. Follow a diet and exercise plan that’s healthy for you.
6. Use a cane or walker if you have difficulty walking or have an increased risk for falls.
How Is Osteoporosis Diagnosed?
A healthcare provider will diagnose osteoporosis with a bone density test. A bone density test is an imaging test that measures the strength of your bones. It uses X-rays to measure how much calcium and other minerals are in your bones.
Healthcare providers sometimes refer to bone density tests as DEXA scans, DXA scans or bone density scans. All of these are different names that refer to the same test.
A bone density test uses low levels of X-rays to measure the density and mineral content of your bones. It’s similar to a typical X-ray. It’s an outpatient procedure, which means you won’t have to stay in the hospital. You can go home as soon as you finish your test. There are no needles or injections in this test.
Checking for changes in your bone density is the best way to catch osteoporosis before it causes a bone fracture. Your provider might suggest you get regular bone density tests if you have a family history of osteoporosis, if you’re over 50, or you have osteopenia.
Treatment for Osteoporosis
Your healthcare provider will suggest a combination of treatments that slow down your bone loss and strengthen your existing bone tissue. The most important part of treating osteoporosis is preventing bone fractures.
The most common osteoporosis treatments include:
1. Exercise: Regular exercise can strengthen your bones (and all the tissue connected to them, like your muscles, tendons and ligaments). Your provider might suggest weight-bearing exercise to strengthen your muscles and train your balance. Exercises that make your body work against gravity like walking, yoga, Pilates and tai chi can improve your strength and balance without putting too much stress on your bones. You might need to work with a physical therapist to find exercises and movements that are right for you.
2. Vitamin and mineral supplements: You might need over-the-counter or prescription calcium or vitamin D supplements. Your provider will tell you which type you need, how often you should take them and which dosage you’ll need.
3. Medications for osteoporosis: Your provider will tell you which prescriptions will work best for you and your body. Some of the most common medications providers use to treat osteoporosis include hormone therapies like replacement estrogen or testosterone and bisphosphonates. People with severe osteoporosis or a high risk of fractures might need medications, including parathyroid hormone (PTH) analogs, denosumab and romosozumab. These medications are usually given as injections.
When should I go to the ER?
Go to the emergency room if you think you have a broken bone or if you experience any of the following symptoms:
1. Intense pain.
2. You can’t move a part of your body.
3. A part of your body is noticeably different looking or out of its usual place.
4. You can see your bone through your skin.
5. Swelling.
6. New bruising that appears at the same time as any of these other symptoms.
Complications
Bone breaks, particularly in the spine or hip, are the most serious complications of osteoporosis. Hip fractures often are caused by a fall and can result in disability and even an increased risk of death within the first year after the injury.
In some cases, broken bones in the spine can occur even if you haven't fallen. The bones that make up your spine, called vertebrae, can weaken to the point of collapsing, which can result in back pain, lost height and a hunched-forward posture.
Frequently Asked Questions About Osteoporosis
You should expect to manage osteoporosis for a long time, usually the rest of your life. You’ll need regular appointments with a healthcare provider and bone density tests. Your provider will monitor any changes in your bone density and will adjust your treatments as needed.
Visit a healthcare provider if you notice any changes in your body that might be osteoporosis warning signs. Tell your provider about any other symptoms you’re experiencing, especially if you have bone pain or trouble moving.
Following a diet and exercise plan that’s healthy for you will help you maintain your bone (and overall) health. See a healthcare provider for regular checkups. They’ll also help catch any issues or symptoms that affect your bones as soon as possible.
Osteoporosis itself isn’t fatal and won’t change your life expectancy (how long you’ll live). But it can make you more likely to experience a bone fracture (and can increase your risk of more severe breaks or complications from a fracture). Some studies have found that hip fractures in adults older than 65 lead to reduced mobility and an earlier death.