An overview of Arthritis
What is Arthritis?
Arthritis is the swelling and tenderness of one or more joints.
Arthritis is a disease that affects your joints (areas where your bones meet and move). Arthritis usually involves inflammation or degeneration (breakdown) of your joints.
The word “arthritis” means “joint inflammation.” However, inflammation may also affect the tendons and ligaments surrounding the joint. The symptoms can develop gradually or suddenly and may impair a person’s ability to perform everyday tasks.
Type of Arthritis
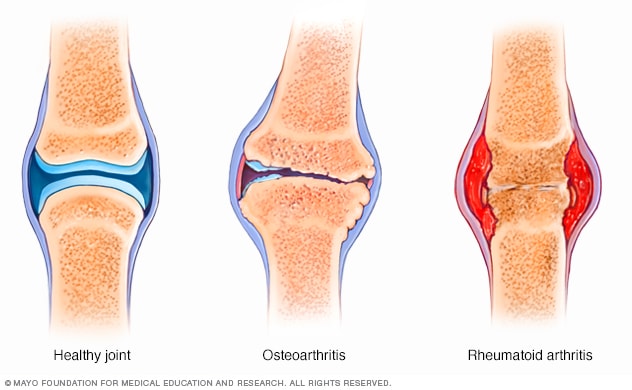
Rheumatoid arthritis : a disease that causes the immune system to attack synovial membranes in your joints.
Osteoarthritis : or “wear and tear” arthritis, which develops when joint cartilage breaks down from repeated stress. It’s the most common form of arthritis.
Ankylosing spondylitis : or arthritis of the spine (usually your lower back).
Juvenile arthritis (JA) : a disorder where the immune system attacks the tissue around joints. JA typically affects children 16 or younger.
Gout : a disease that causes hard crystals of uric acid to form in your joints.
Psoriatic arthritis : joint inflammation that develops in people with psoriasis (autoimmune disorder that causes skin irritation).
Septic arthritis is a joint inflammation that results from a bacterial or fungal infection. It commonly affects the knee and hip. It typically affects 2-6 people 100,000.
Causes of Arthritis
Different types of arthritis have different causes. For instance, gout is the result of too much uric acid in your body.
Osteoarthritis involves wear-and-tear damage to a joint's cartilage — the hard, slick coating on the ends of bones where they form a joint. Cartilage cushions the ends of the bones and allows nearly frictionless joint motion, but enough damage can result in bone grinding directly on bone, which causes pain and restricted movement. This wear and tear can occur over many years, or it can be hastened by a joint injury or infection.
In rheumatoid arthritis, the body's immune system attacks the lining of the joint capsule, a tough membrane that encloses all the joint parts. This lining (synovial membrane) becomes inflamed and swollen. The disease process can eventually destroy cartilage and bone within the joint.
Other possible causes may include:
1. an injury, which can lead to degenerative arthritis
2. an abnormal metabolism, which can cause gout and calcium pyrophosphate deposition disease (CPPD)
3. a genetic inheritance, which can lead to developing osteoarthritis
4. an infection such as Lyme disease, which can trigger arthritis symptoms
5. an immune system dysfunction, such as the type that causes RA and lupus
Signs and symptoms of Arthritis
Different types of arthritis have different symptoms. They can be mild in some people and severe in others. Joint discomfort might come and go, or it could stay constant. Common symptoms include:
1. Pain.
2. Redness.
3. Stiffness.
4. Swelling.
5. Tenderness.
6. warmth
How can arthritis be prevented?
You can lower your chances of developing arthritis by:
1. Avoiding tobacco products.
2 .Doing low-impact, non-weight bearing exercise.
3. Maintaining a healthy body weight.
4. Reducing your risk of joint injuries.
How is arthritis diagnosed?
If you think you may have arthritis, see your healthcare provider. The provider will ask about your symptoms and learn how joint pain affects your life. Your provider will perform a physical exam, which may include:
1. Assessing mobility and range of motion in your joints.
2. Checking for areas of tenderness or swelling around your joints.
3. Evaluating your overall health to determine if a different condition could be causing your symptoms.
How is arthritis treated?
There’s no cure for arthritis, but there are treatments that can help you manage the condition. Your treatment plan will depend on the severity of the arthritis, its symptoms and your overall health.
Conservative (nonsurgical) treatments include:
1. Medication: Anti-inflammatory and pain medications may help relieve your arthritis symptoms. Some medications, called biologics, target your immune system’s inflammatory response. A healthcare provider may recommend biologics for your rheumatoid or psoriatic arthritis.
2. Physical therapy: Rehabilitation can help improve strength, range of motion and overall mobility. Therapists can teach you how to adjust your daily activities to lessen arthritic pain.
3. Therapeutic injections: Cortisone shots may help temporarily relieve pain and inflammation in your joints. Arthritis in certain joints, such as your knee, may improve with a treatment called viscosupplementation. It injects lubricant to help joints move smoothly.
For Surgical procedures
Healthcare providers usually only recommend surgery for certain severe cases of arthritis. These are cases that haven’t improved with conservative treatments. Surgical options include:
1. Fusion: Two or more bones are permanently fused together. Fusion immobilizes a joint and reduces pain caused by movement.
2. Joint replacement: A damaged, arthritic joint gets replaced with an artificial joint. Joint replacement preserves joint function and movement. Examples include ankle replacement, hip replacement, knee replacement and shoulder replacement.
What’s the outlook for someone living with arthritis?
Since there’s no cure for arthritis, most people need to manage arthritis for the rest of their lives. Your healthcare provider can help you find the right combination of treatments to reduce symptoms. One of the biggest health risks associated with arthritis is inactivity. If you become sedentary from joint pain, you may face a greater risk for cancer, heart disease, diabetes and other serious conditions.
What can I do to make living with arthritis easier?
Changing your routine can make living with arthritis easier. Adjust your activities to lessen joint pain. It may help to work with an occupational therapist (OT). An OT is a healthcare provider who specializes in managing physical challenges like arthritis.
An OT may recommend:
1. Adaptive equipment, such as grips for opening jars.
2. Techniques for doing hobbies, sports or other activities safely.
3. Tips for reducing joint pain during arthritic flare-ups.
Risk factors of Arthritis?
Risk factors for arthritis include:
1. Family history. Some types of arthritis run in families, so you may be more likely to develop arthritis if your parents or siblings have the disorder.
2. Age. The risk of many types of arthritis — including osteoarthritis, rheumatoid arthritis and gout — increases with age.
3. Your sex. Women are more likely than men to develop rheumatoid arthritis, while most of the people who have gout, another type of arthritis, are men.
4. Previous joint injury. People who have injured a joint, perhaps while playing a sport, are more likely to eventually develop arthritis in that joint.
5. Obesity. Carrying excess pounds puts stress on joints, particularly your knees, hips and spine. People with obesity have a higher risk of developing arthritis.
Frequently Asked Questions About Arthritis
Nearly 40 million Americans or one in every seven people have arthritis. It affects people of all ages but it most often comes on as a person gets older.
Numbness is often a symptom of nerve involvement. For instance, numbness in the arm may be related to nerve irritation in the neck. In such a situation, turning or bending the head to the involved side may increase the symptoms. For example, a pinched nerve in the right side of the neck may cause numbness in the arm and hand when a person attempts to look back over the right shoulder. If nerve irritation becomes more severe, the arm and hand may become weak. A physical examination X-rays and an MRI of the neck and electrodiagnostic tests may be useful in establishing the diagnosis.
Yes, children can get arthritis. The most common type of arthritis found in children is juvenile idiopathic arthritis (JIA), also known as childhood arthritis or juvenile rheumatoid arthritis.
It’s normal to have some pain, stiffness, and swelling after starting a new physical activity program. It may take 6 to 8 weeks for your joints to get used to your new activity level, but sticking with your activity program will result in long-term pain relief.