An overview of Diverticular Disease
What is Diverticular Disease?
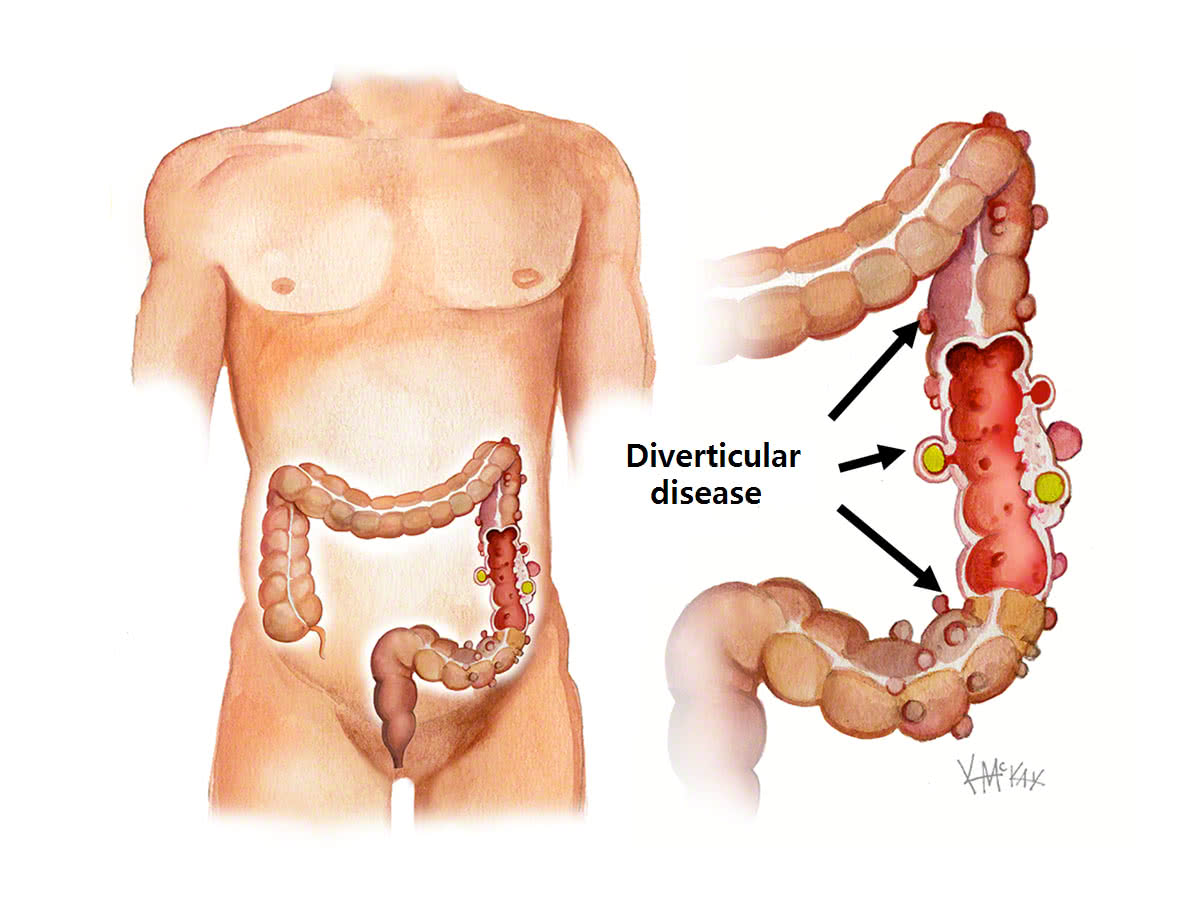
Diverticula are small, bulging pouches that can form in the lining of your digestive system. They are found most often in the lower part of the large intestine (colon). Diverticula are common, especially after age 40, and seldom cause problems.
Diverticular disease consists of three conditions that involve the development of small sacs or pockets in the wall of the colon, including diverticulosis, diverticular bleeding, and diverticulitis.
Diverticulosis
The presence of diverticula is known as diverticulosis (die-vur-tik-yoo-LOE-sis). When one or more of the pouches become inflamed, and in some cases infected, that condition is known as diverticulitis (die-vur-tik-yoo-LIE-tis). Diverticulitis can cause severe abdominal pain, fever, nausea and a marked change in your bowel habits.
Diverticulitis
Diverticulitis occurs when there is inflammation and infection in one or more diverticula. This usually happens when outpouchings become blocked with waste, allowing bacteria to build up, causing infection.
Diverticular Bleeding
Diverticular bleeding occurs with chronic injury to the small blood vessels that are next to the diverticula.
Causes of Diverticula and Diverticulitis
Diverticula usually develop when naturally weak places in your colon give way under pressure. This causes marble-sized pouches to protrude through the colon wall.
Diverticulitis occurs when diverticula tear, resulting in inflammation, and in some cases, infection.
Signs and symptoms of diverticulitis
1. Pain, which may be constant and persist for several days. The lower left side of the abdomen is the usual site of the pain. Sometimes, however, the right side of the abdomen is more painful, especially in people of Asian descent.
2. Nausea and vomiting.
3. Fever.
4. Abdominal tenderness.
5. Constipation or, less commonly, diarrhea.
How Can Diverticulosis Be Prevented?
There’s no way to prevent Crohn’s disease. These healthy lifestyle changes can ease symptoms and reduce flare-ups:
To prevent diverticular disease or reduce the complications from it, maintain good bowel habits. Have regular bowel movements and avoid constipation and straining. Eating appropriate amounts of the right types of fiber and drinking plenty of water and exercising regularly will help keep bowels regulated.
The American Dietetic Association recommends 20 to 35 grams of fiber a day. Every person, regardless of the presence of diverticula, should try to consume this much fiber every day. Fiber is the indigestible part of plant foods. High-fiber foods include whole grain breads, cereals, and crackers; berries; fruit; vegetables, such as broccoli, cabbage, spinach, carrots, asparagus, squash, and beans; brown rice; bran products; and cooked dried peas and beans, among other foods.
How is Diverticulosis and Diverticulitis diagnosed?
How Is Diverticulosis Diagnosed?
Because people with diverticulosis do not have any symptoms, it is usually found through tests ordered for an unrelated reason. They usually include barium enema, sigmoidoscopy and colonoscopy.
How Is Diverticulitis Diagnosed?
If you are experiencing the symptoms of diverticulitis, it is important to see your doctor.
Your doctor will ask questions about your medical history (such as bowel habits, symptoms, diet, and current medications) and perform a physical exam, possibly including an abdominal exam.
One or more diagnostic tests may be ordered. Tests usually include blood tests and CT scanning.
In people with rapid, heavy rectal bleeding, the doctor may order a colonoscopy to locate the source of bleeding.
Treatment
How is diverticulosis treated?
If you have diverticulosis, you likely don’t have symptoms and don’t need treatment. However, since diverticulosis could lead to diverticulitis, you should eat a diet high in fiber as a preventive measure. This means eating more fruits, vegetables, grains, nuts, seeds, beans, legumes and less red meat.
How is diverticulitis treated?
If your diverticulitis is mild, your healthcare provider will prescribe an oral antibiotic, such as metronidazole (Flagyl®), trimethoprim-sulfamethoxazole (Bactrim®), ciprofloxacin (Cipro®) or amoxicillin and clavulanic acid (Augmentin®). Rest, taking over-the-counter medications for pain and following a low-fiber diet or a liquid diet may be recommended until your symptoms improve. Once your symptoms improve, you can slowly return to soft foods, then a more normal diet, which should be one that includes many high-fiber foods. You and your healthcare provider will discuss the specifics of your treatment plan.
If your diverticulitis is severe, you have rectal bleeding or are having a repeat bout of diverticulitis, you may be admitted to the hospital to receive intravenous (IV) antibiotics, IV fluids or possibly be considered for surgery.
What should I expect if I have been diagnosed with diverticular disease?
If you’ve been told you have diverticulosis, this is usually not cause for concern. This condition is very common and increases with age. It is present in about 50% of people over age 60 and in almost everyone over age 80. You likely won’t even have symptoms if you have diverticulosis. If you have a mild case of diverticulosis, it may go away on its own without treatment.
Up to 30% of people with diverticulosis do develop diverticulitis. Between 5% and 15% will develop rectal bleeding.
Most people who have diverticulitis will recover with about a seven to 10-day course of antibiotics and rest. Severe complication of diverticulitis occur in about the following percent of people: perforation of the colon (1% to 2% of patients), obstruction (rare), fistula (14%) or abscess (30%).
The best self-treatment is to eat a high-fiber diet (one filled with fruits and vegetables, cereals and whole grains, nuts, beans and legumes. Also, drink more fluids (half your body weight in ounces each day) and exercise (helps speed waste through your colon).
Frequently Asked Questions About Diverticular Disease
Diverticulitis can be treated and be healed with antibiotics. Surgery may be needed if you develop complications or if other treatment methods fail and your diverticulitis is severe. However, diverticulitis is generally considered to be a lifelong condition.
If the affected area of your colon is removed, another surgery is usually not needed. The most common location for diverticulitis is the sigmoid colon, which is the S-shaped near end portion of your colon. Although this is the most common location, it’s possible for diverticula to form in other areas of your colon. Because each person is different, be sure to ask your healthcare provider, surgeon, or colon specialist about your risk for return appearance of diverticulitis.
Yes, you can take a fiber supplement. Available products include FiberCon®, Citrucel®, Metamucil® and generics of these branded products and other fiber products. Be sure to drink at least 8 ounces of liquids with your supplement.
Diverticulosis is very common in Western populations and occurs in 10% of people over age 40 and in 50% of people over age 60. The rate of diverticulosis increases with age, and it affects almost everyone over age 80.