An overview of Liver Cancer
What is Liver Cancer?
Cancer that starts in your liver's cells is called liver cancer. Your liver, an organabout the size of a football, is located in the upper right part of your abdomen,above your stomach and below your diaphragm.
The liver is prone to developing a number of cancers. Hepatocellular carcinoma, themost prevalent form of liver cancer, develops in the primary liver cell type(hepatocyte). Hepatoblastoma and intrahepatic cholangiocarcinoma are twosignificantly less frequent kinds of liver cancer.
Cancer that spreads to the liver is more common than cancer that begins in the livercells. Cancer that begins in another area of the body — such as the colon, lung orbreast — and then spreads to the liver is called metastatic cancer rather than livercancer. This type of cancer is named after the organ in which it began — such asmetastatic colon cancer to describe cancer that begins in the colon and spreads tothe liver.
What are the liver cancer stages?
Healthcare providers stage HCC using standards set by the Barcelona Clinic LiverCancer system (BCLC). This system evaluates HCC liver on characteristics, includingwhether your liver is working well, tumor size and your symptoms. Healthcareproviders may use different terms for each BCLC stage; sometimes, presented as beingstages I to IV or 0-C or by terms such as early and advanced stage HCC.Hepatocellular carcinoma stages include the following:
Stage I/very early stage/stage 0 : You have a single tumor in your liver thatmeasures less than 2 centimeters (cm). Blood tests show your bilirubin level isnormal.
Stage II/early stage/stage A : You have a single tumor that measures 5 cm orless or you have more than one tumor that measures less than 3 cm. The tumor mayhave spread to your blood vessels.
Stage III/intermediate stage/stage B : In this stage, you may have more thanone tumor and/or a tumor that measures more than 5 cm. The tumor may have spread toyour lymph nodes, large blood vessels or another organ.
Stage IV/advanced stage/stage C : The cancer has spread to other places inyour body, such as your lungs or bones, as well as lymph nodes.
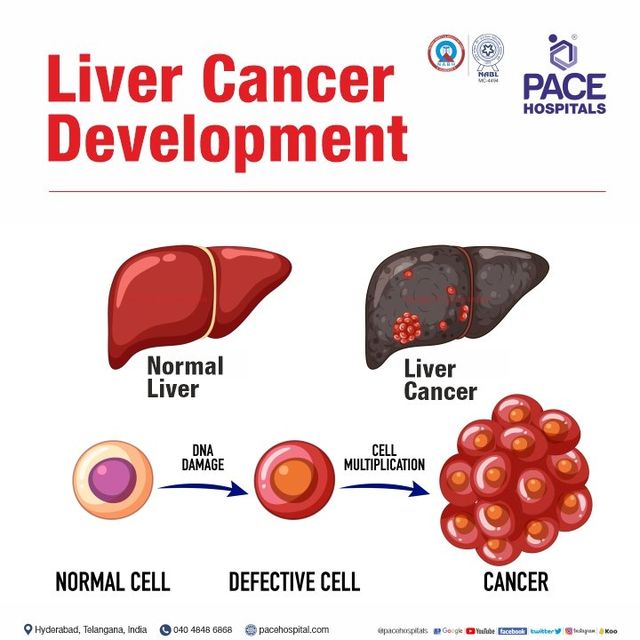
What causes liver cancer?
When something alters the DNA of healthy liver cells, liver cancer results. The genesthat instruct our cells how to function are carried by DNA. Everyone has genes thatcontrol when cells divide, proliferate, and die. Oncogenes, for instance, promotecell division and growth. Other genes, known as tumor suppressor genes, keep an eyeon cell activity, preventing uncontrollable cell growth and ensuring that cells passaway when they should.
Our cells receive new instructions whenever our DNA is altered or mutated. DNAalterations in HCC activate oncogenes and/or silence tumor suppressor genes. Forinstance, research indicates that more than half of all instances of HCC are causedby cirrhosis brought on by the hepatitis B and C viruses. These viruses modify theDNA of the liver cells they infect, transforming normal liver cells into malignantones.
Signs and symptoms of liver cancer
Most people don't have signs and symptoms in the early stages of primary livercancer. When signs and symptoms do appear, they may include:
1. Losing weight without trying
2. Loss of appetite
3. Upper abdominal pain
4. Nausea and vomiting
5. General weakness and fatigue
6. Abdominal swelling
7. Yellow discoloration of your skin and the whites of your eyes (jaundice)
8. White, chalky stools
How can I prevent liver cancer?
While you can’t completely prevent liver cancer, you can do the following to loweryour chances of getting liver cancer:
1. Avoid behaviors that lead to cirrhosis.
2. Reach or maintain a healthy weight.
3. Get a hepatitis B vaccine. This vaccine is safe for nearly everyone. Ask yourdoctor about the hepatitis A vaccine.
4. Avoid hepatitis C.
5. If you have any liver disease, have diabetes, obesity or are a heavy drinker, askyour healthcare provider about liver cancer screenings.
How is liver cancer diagnosed?
Your healthcare provider may suspect you have liver cancer if they find liver cancersigns and symptoms during your physical examination. They may order the followingtests to learn more:
Ultrasound (sonography) : This test provides pictures of your soft tissuestructures. Healthcare providers use ultrasound to look for liver tumors.
Blood tests : Healthcare providers may do blood tests for cancer, such as aliver function test, to check on liver enzymes, proteins and other substances thatshow whether your liver is healthy or damaged. They may test for alfa-fetoprotein(AFP). High AFP levels may indicate liver cancer.
Computed tomography (CT) scan : This special type of X-ray takes detailedimages of your liver, providing information about liver tumor size and location.
Magnetic resonance imaging (MRI) : This test produces very clear images ofyour body using a large magnet, radio waves and a computer.
Angiogram : This test helps healthcare providers examine your liver’s bloodvessels. During this test, your healthcare provider injects dye into an artery sothey can track blood vessel activity and look for blockages.
Biopsy : Healthcare providers remove liver tissue to look for signs of cancer.Biopsies are the most reliable way to confirm a liver cancer diagnosis.
How is liver cancer treated?
Surgically removing a portion of your liver, liver transplantation, andliver-directed therapies including hepatic arterial embolization and ablation are afew of the primary treatments offered by healthcare providers for HCC and IHC.Moreover, they might use different kinds of chemotherapy, chemoembolization,radiation therapy, radioembolization, immunotherapy, and targeted therapy.
Frequently Asked Questions About liver cancer
No, it’s not common, but liver cancer cases aresteadily increasing. Healthcare providers estimate about 1% ofall men and women in the United States will be diagnosed with aform of liver cancer during their lifetime.
HCC and IHC affect more men than women and are mostoften diagnosed between the ages of 55 and 64. People whose raceincludes Asian/Pacific Islander, Hispanic or AmericanIndian/Alaskan Indian are more likely to develop primary livercancer than people who are Black or white.
Successful liver transplants can cure liver cancer,but not everyone who needs a liver transplant will be healthyenough to go through a transplant or able to find a donor.Studies show people who have surgery to remove part of theirliver tend to live longer than people whose illness preventssurgery. When that happens, healthcare providers focus ontreatments to help people live with quality of life for as longas possible.
Liver cancer and liver cancer treatments take a tollon your body. Some people have liver transplants or surgery toremove part of their liver. Other people may need treatment foras long as they live. Either way, you should plan on regularappointments with your healthcare provider so they can monitoryour progress and watch for signs of recurring liver cancer(cancer that comes back). For example, people who don’t havesigns of liver cancer after treatment should plan on follow-upimaging and blood tests every three to six months for the firsttwo years after treatment.